Clinical Psychology and Special Education
2022. Vol. 11, no. 2, 158–173
doi:10.17759/cpse.2022110210
ISSN: 2304-0394 (online)
Gold Standard Versus Treatment as Usual: Assessment Practices in the Juvenile Justice System
Abstract
Mental health concerns are highly prevalent in the juvenile justice system (JJS). Assessment practices vary significantly across probation departments, often relying on past medical history or unstructured clinical interviews. Numerous structured and semi-structured assessment tools exist, some of which have previously been used within JJS samples. The current research compared mental health diagnosis prevalence and distribution as assigned by the current practice in a probation department versus utilizing the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) in a sample of youth involved with the JJS. Results suggested the K-SADS identified a higher variety of mental health concerns with higher precision (e.g., all diagnoses were specified rather than unspecified). However, the standard assessment practice identified a higher prevalence of ADHD diagnoses, as well as “Other Conditions That May Be a Focus of Clinical Attention.” Limitations and future directions are discussed.
General Information
Keywords: assessment, juvenile justice, K-SADS, mental health, delinquency, semi-structured assessment
Journal rubric: Methods and Techniques
Article type: scientific article
DOI: https://doi.org/10.17759/cpse.2022110210
Funding. The preparation of this article was supported by P20 HD091005 (Principal investigator: Elena L. Grigorenko) funded by Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD).
Acknowledgements. We thank Harris County Juvenile Probation Department (HCJPD) for providing access to their administrative data. We also thank Sascha Hein, Ph.D., for securing and coordinating the data provided by HCJPD, as well as his feedback on the draft of the manuscript.
Received: 01.05.2022
Accepted:
For citation: Kovalenko J.D., Li N., Grigorenko E.L. Gold Standard Versus Treatment as Usual: Assessment Practices in the Juvenile Justice System [Elektronnyi resurs]. Klinicheskaia i spetsial'naia psikhologiia = Clinical Psychology and Special Education, 2022. Vol. 11, no. 2, pp. 158–173. DOI: 10.17759/cpse.2022110210.
Full text
It is well-established that many youths involved with the juvenile justice system (JJS) face significant mental health concerns, with estimates of prevalence of mental illness ranging from 65–98% [3; 13; 14; 17; 36; 41]. Frequent diagnoses include disruptive behavior disorders (DBDs), substance use disorders, ADHD, and affective disorders, which are more prevalent in girls [17; 37]. A proper diagnosis carries important practical implications. Specifically, assigning a diagnosis can provide a better understanding of the youth’s problems and needs, which in turn may ensure they receive appropriate treatment. As such, clinicians should be very careful when assigning a diagnosis to a youth because that diagnosis not only impacts the type of intervention to be provided but also may bias how judges and probation officers view the juveniles [14]. Thus, reliable and valid diagnoses are particularly important in a forensic setting.
A report from the Office of Juvenile Justice and Delinquency Prevention (OJJDP) suggests that there are highly variable assessment practices within the JJS, and there is
a reliance on the youth’s past utilization of mental health services as an indicator of the youth’s current problems [41]. Authors reported that a common practice to evaluate mental health needs is to rely on the history of receiving prior mental health services, which is not always reliable or reflective of the youth’s current needs. A reliable, valid but also cost-effective way of diagnosing youth within the system is necessary to ensure youth receive the services they need. Structured or semi-structured diagnostic interviews would be a suitable tool within the JJS due to their validity, reliability, and ability for non-clinicians to administer it (including computerized self-administration).
Structured interviews and psychological tests provide empirically quantified information, are often normed, and have research on the reliability and validity of that specific individual test or assessment [29]. Thus, clinicians have a clearer opportunity to gauge the data they are collecting from the individual [29]. Studies have found that when psychiatrists were treating patients who received a structured interview (Structured Clinical Interview for DSM Disorders, SCID) compared with control patients (who received treatment as usual, which included review of service eligibility, a clinical interview, chart review, and laboratory tests), they were more likely to not only update and change the diagnosis consistent with the SCID results but to order additional evaluative procedures, change prescription medication type while being less likely to increase patients' medication dosages [20].
Structured diagnostic interviews are often more reliable than unstructured clinical interviews due to the questions being standardized, thus resulting in decreased variability among interviewers, less variability of the symptoms over time, as well as reliability between client self-report and collateral information [35; 39]. Structured interviews also have increased validity because they cover diagnostic criteria systematically and completely, some of which may be overlooked during less formal evaluation procedures [28; 34].
Structured diagnostic tools are cost-effective, as they can be administered by non-clinicians or clinicians still in training. Some semi-structured interviews are computerized and even offer self-administration options, such as the Kiddie Schedule for Affective Disorders and Schizophrenia, KSADS-COMP [21; 38]. According to the Kennedy Krieger Institute, the K-SADS is the most widely used and well validated diagnostic interview for children and adolescents [38]. The reliability and validity of the K-SADS-COMP are well-documented and are convergent between a clinician-administered version, a self-administered youth version, and a self-administered parent version [38].
A number of structured and semi-structured diagnostic interviews have been used in the JJS, including the K-SADS [5; 26]. Other assessments included the Practical Adolescent Dual Diagnosis Interview (PADDI), which identified a high prevalence of mental health concerns in JJS youth (ranging from 92% for male participants to 97% for female participants), provided information on comorbid disorders, and demonstrated strong internal consistency [1; 7]. The Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) has also been used within the community and the JJS to assess mental health concerns and suggested that disruptive disorders were most frequent, followed by substance-related disorders, anxiety, and mood disorders [32].
A meta-analysis provided an overview of the results of additional structured assessment tools, including versions of the Diagnostic Interview Schedule for Children (DISC), Schedules for Clinical Assessment in Neuropsychiatry (SCAN), Diagnostic Interview for Children and Adolescents, Revised (DICA-R), and Salford Needs Assessment Schedule for Adolescents (SNASA) [9]. The results suggested the overall high prevalence of mental health concerns, including ADHD and CD, as well as an increased prevalence of rates of depression in girls. In addition, it was reported that the DISC provided lower prevalence estimates for depression, ADHD, and conduct disorder than other instruments, while studies that utilized psychiatrists as interviewers had lower prevalence estimates of depression [9].
Research studies that have used versions of the K-SADS have reported a number of mental health concerns in the system. For example, T. Kang, J. Wood, J. Eno Louden, and E. Ricks [19] recorded that even among low-risk offenders, mental health services and substance abuse treatment are highly needed. They also observed that girls are in need of more services for affective disorders. Additional studies that utilized the K-SADS identified a high prevalence of non-suicidal self-injury in youth involved with juvenile justice or welfare systems [26]. Research suggests that mental health problems are a significant factor associated with delinquency and that when assessed with the K-SADS, a majority of female juvenile delinquents met lifetime criteria for at least three psychiatric diagnoses [6].
Given the importance of a proper diagnosis for youths involved in the JJS, utilizing a structured or semi-structured interview may provide useful information to the mental health providers in the JJS. A recent study found that in a sample of youth involved with a Texas juvenile probation department, the primary diagnosis from the disruptive behavior chapter of DSM-5 was Unspecified Disruptive, Impulse-Control, and Conduct Disorder(UDICCD) [23]. Based on the literature, that finding was unexpected as specified DBD’s such as oppositional defiant disorder (ODD) or CD were anticipated [23; 37]. While the unspecified category has been reported to be frequently used as a placeholder or reflect other diagnostic uncertainty, there may be treatment implications due to the “vagueness” of the diagnosis [10; 11; 23]. Specifically, treatment and other correctional decisions within the justice system are dependent on the type of presenting concerns the youth has [2], yet Kovalenko and colleagues’ article demonstrated that despite juveniles receiving the same UDICCD diagnosis, they may have different presenting concerns and needs (e.g., academic achievement concerns versus internalizing comorbid diagnoses). A valid and reliable diagnostic system to screen for specific mental health concerns would be beneficial within the JJS as it would provide accurate diagnoses that can be targeted with interventions and can help prevent future recidivism [7].
It has been shown that mental health concerns, including in individuals involved with the JJS, often carry a stigma in the community [18; 33]. A qualitative study found that parents of youth who present mental health concerns and have had contact with the JJS have significant concerns about their youth being “labeled” with a diagnosis due to worries about stigmatization [42]. The article also noted that the youth primarily received services through their involvement with the JJS (e.g., as a component of their probation) rather than the family seeking out services independently. It may be possible that the UDICCD diagnosis is used to minimize stigmatization that is associated with mental illness, however research on the effects of diagnostic labels on the perception of individuals involved with the justice system are mixed. While some studies identified a negative relationship between a diagnostic label and mock juror’s perception of the youth [8], other research did not identify a negative relationship between a diagnostic label and the perception of the youth by judges or juvenile probation officers (JPO). A diagnostic label also did not impact JPO’s recommendations of sanctions, in fact, it only impacted their recommendations for the youth to receive additional psychological services [30; 31].
A semi-structured diagnostic interview would allow for consistent assessment of youth and provide a more accurate picture of the types of problems youths in the JJS face, as well as lead to more targeted interventions. The aim of this study was to investigate the distribution of mental disorders in JJS-involved youth residing in post-adjudication facility and in their communities using a semi-structured diagnostic interview and compare to the prevalence of disorders given current practice. In particular, we hypothesized that the semi-structured diagnostic interview would provide valid and reliable results on the distribution of mental disorders in a sample of JJS youth as the K-SADS is the “gold standard” of mental health assessments. In addition, we hypothesized that the distribution and prevalence of diagnoses from this study would differ from the distribution and prevalence of diagnoses identified with the current practice in HCJPD. Specifically, with the semi-structured tool more specified as compared to unspecified diagnoses will be identified.
Method
The study aimed to use a semi-structured diagnostic tool to provide valid and reliable diagnoses to JJS youth involved with the Harris County Juvenile Probation Department (HCJPD). HCJPD maintains a centralized database for youth under their jurisdiction. As part of a collaborative project, HJCPD provided access to the data of youth who participated in the current research study.
Participants
Youth placed in HCJPD detention facilities or those who are on probation were invited to participate in the current research study by HCJPD social workers or JPO’s. The social workers or JPO’s obtained all necessary documentation from parents/legal guardians with regard to their children, including informed consent for participation in the research study. Criteria for involvement included conversational English proficiency. Data were collected in person or over Zoom, depending on the youth’s placement. Due to the ongoing Covid-19 health crisis, very few youths were placed within post-adjudicated detention facilities.
For youth who have had a K-SADS assessment completed, HCJPD provided additional data. As noted above, not every juvenile on probation receives a full behavioral health evaluation. Specifically, to limit unnecessary exposure to the JJS, full behavioral health evaluations are primarily collected on youth who have been placed in detention facilities. No youth in our sample who were on probation had behavioral health data available from HJCPD. Thus, the sample of youth who had both K-SADS and HCJPD data was primarily comprised of youth who were placed within post-adjudicated facilities, which potentially skewed the matched sample to represent more youth who have been in detention.
A total of n=27 youth from the probation department and post-adjudicated facilities participated in the K-SADS assessment. Three youth had assessments that were initiated; however, they were not completed (and did not have enough information for a diagnosis), thus they were not included in either K-SADS-only analyses or in the comparison analyses with HCJPD data. The overall K-SADS sample size included in descriptive analyses was n=24 (Mage=15.6, SD=0.89;83.3% male). HCJPD was unable to provide data on seven youth from the K-SADS sample as they did not have behavioral health evaluations. Four of the seven unmatched youth were on probation rather than in a detention facility. The sample used in analyses to compare HCJPD and K-SADS data were 16 youth (Mage=15.8, SD=0.93; 87.5% male). Data on race/ethnicity were only available for youth who were matched with HCJPD data as it was not collected as part of the K-SADS study. The racial distribution included Black/African American youth (43.8%) and Hispanic/Latinx youth (56.3%). Demographic information is provided in Table 1 for the 16 youth who had K-SADS and HCJPD data.
Table 1
Demographics and number of unspecified diagnoses for matched sample
|
Youth |
Age |
Gender |
Race |
N of unspecified diagnoses |
|
|
1 |
16 |
Male |
Black |
0 |
1 |
|
2 |
17 |
Male |
Black |
0 |
0 |
|
3 |
16 |
Male |
Black |
0 |
1 |
|
4 |
15 |
Male |
Hispanic |
0 |
0 |
|
5 |
14 |
Male |
Hispanic |
0 |
0 |
|
6 |
15 |
Male |
Hispanic |
0 |
0 |
|
7 |
16 |
Male |
Black |
0 |
2 |
|
8 |
15 |
Female |
Black |
0 |
0 |
|
9 |
17 |
Male |
Hispanic |
0 |
2 |
|
10 |
16 |
Male |
Hispanic |
0 |
1 |
|
11 |
15 |
Male |
Hispanic |
0 |
0 |
|
12 |
15 |
Male |
Black |
0 |
3 |
|
13 |
17 |
Male |
Hispanic |
0 |
0 |
|
14 |
16 |
Female |
Hispanic |
0 |
1 |
|
15 |
15 |
Male |
Hispanic |
0 |
1 |
|
16 |
17 |
Male |
Black |
0 |
0 |
Assessments
HCJPD Procedures. Information on youth’s diagnoses in the dataset is dependent on whether a youth received a full behavioral health evaluation or a screener. Screeners utilize an unstructured diagnostic interview and sometimes academic achievement and IQ assessments as needed. Full evaluations utilize an unstructured diagnostic interview and follow up questionnaires for specific concerns (mood, ADHD). When available, collateral information (e.g., school records, caregiver report) is incorporated into case conceptualization. All youth within HCJPD receive a screener; however, much fewer youth receive a full behavioral evaluation. HCJPD provided diagnostic information on youth who participated in the K-SADS evaluation; however, as described above, there were seven youth who participated in the K-SADS evaluation who did not have diagnoses assigned by HJCPD and thus were not included in the comparison sample. HCJPD utilizes the DSM-5 nomenclature to assign mental health diagnoses to youth. Of note, HCJPD also provides information on “Other Conditions That May Be a Focus of Clinical Attention,” unlike the K-SADS.
Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS-COMP), clinician administered. The computerized version of the K-SADS uses pre-programmed branching logic, which guides the clinician (or patient) appropriately through the interview. It ensures that all required probes and supplements are administered. In addition, data are automatically stored in an electronic database, eliminating the need for scoring and data entry, thus removing the possibility of human errors [38]. The reliability and validity of the KSADS-COMP are well-documented and are convergent between a clinician-administered version, a self-administered youth version, and a self-administered parent version [37]. Of particular interest, it was reported that for the clinician administered KSADS-COMP, all raters scored 94–96% of items identically, and there was a 98% agreement if the items were above the clinical threshold [38]. In addition, the authors reported correlations between the KSADS-COMP and standardized symptom measures ranging from 0.55 (for bipolar disorder) to 0.76 (for ADHD). The K-SADS provides both current diagnoses (symptoms present in the past two weeks), current diagnoses in partial remission, as well as past diagnoses (meaning the youth endorsed experiencing symptoms in their lifetime) [38].
Data analysis. We completed analyses on two sets of data. The first included all youth assessed via the K-SADS (n=24), with data on current and past diagnoses for the youth. The second sample only included youth who had both K-SADS and HCJPD data available (n=16) from the full K-SADS sample. If youth had numerous evaluations conducted during their time at HCJPD, the latest HCJPD evaluation was used in analyses to ensure the most up-to-date diagnostic information was included. The prevalence of diagnoses and their comorbidities were examined amongst the full K-SADS sample as well as the matched K-SADS/HCJPD sample to identify common mental health difficulties youth in the system face. Diagnoses were grouped based on their chapter in the DSM-5, such as DBD’s anxiety, depression, or bipolar and related disorders. Each youth received a total score for how many diagnoses they received, either via the K-SADS or HCJPD mental health practitioner’s evaluation. The number of unspecified diagnoses were also summed for each youth to examine the prevalence of unspecified diagnoses in youth assessed with K-SADS as compared to prevalence based on the assessment by HCJPD. The ICC statistic was utilized to examine inter-rater reliability and consistency of HCJPD and K-SADS diagnoses. The general guidelines indicate that 0.5 are indicative of poor reliability, while values between 0.75 and 0.9 suggest good reliability [22]. The ICC estimate may be negative in cases where the value of the mean square for error exceeds the mean square for subjects [28]. Figures and tables are provided for variables that could not be statistically analyzed. Analyses were conducted using SPSS.
Results
The average number of current diagnoses (diagnoses at time of testing) provided by the K-SADS for the full sample was just under five (M=4.96; min=0, max=13). The average number of past diagnoses was 2.5 (min=0, max=7). The K-SADS assigned only one unspecified diagnosis for the whole sample. See Figure 1 and for the distribution of current and past diagnoses for the full sample of youth. Substance-related concerns were the most frequently encountered under current diagnoses, accounting for 40% of diagnoses. DBD’s accounted for 17% of the diagnoses within the sample, while anxiety disorders and trauma-and stressor-related disorders were equivalent to 7% each. Of note, the K-SADS identified
a high frequency of homicidal ideation, in particular, in the past diagnoses, as well as suicidality in both current and past diagnoses. For past diagnoses, anxiety and substance-related disorders accounted for 24% and 18%, respectively, of all diagnoses. Only one youth had one unspecified diagnosis in the full sample.
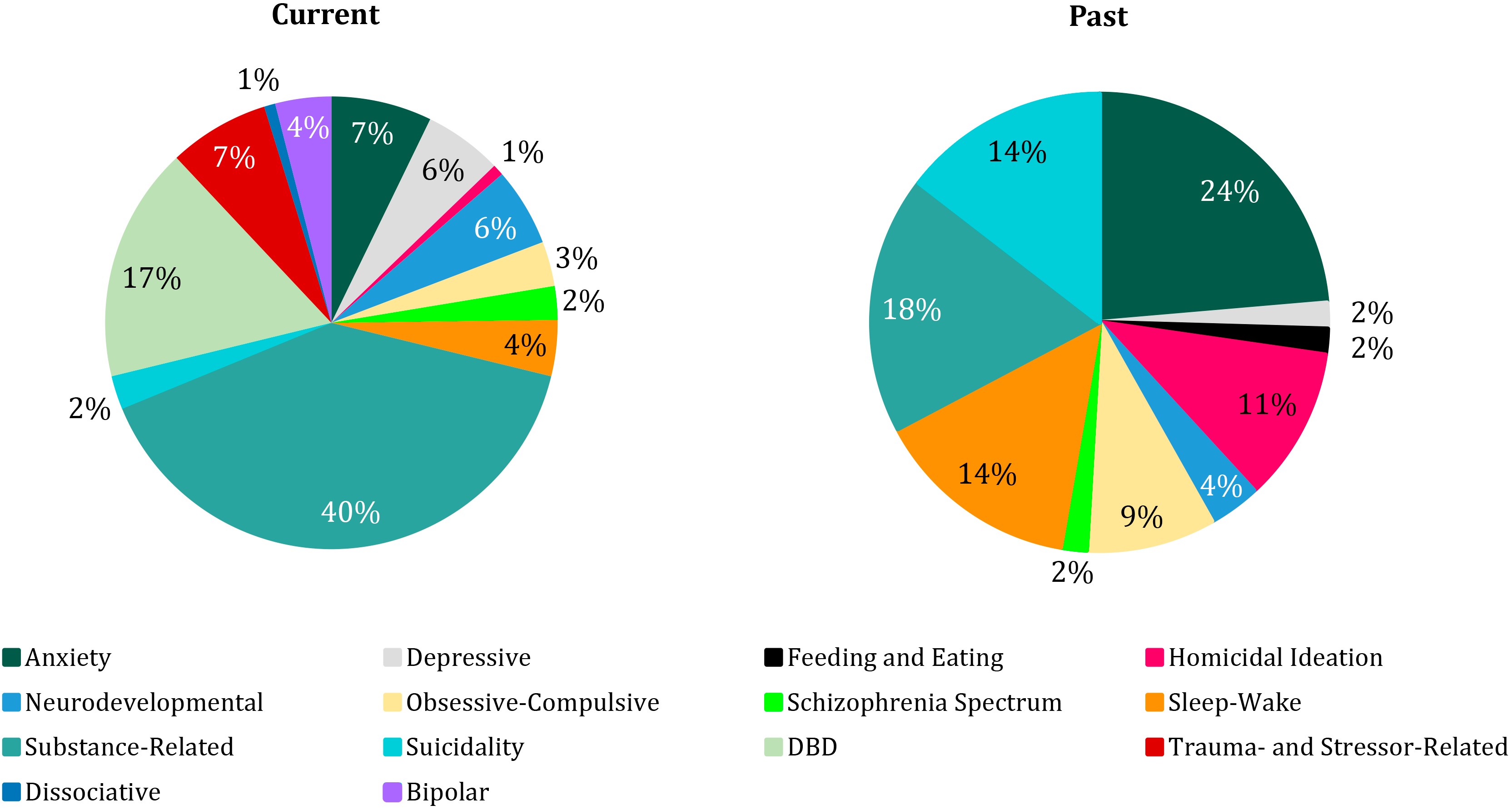
Figure 1. Current and Past K-SADS Diagnosis Prevalence for Full Sample of 24 Youth
For the comparison sample (youth who had both K-SADS and HCJPD data available), the ICC statistic was utilized to determine the consistency of inter-rater reliability of the total sums of diagnoses assigned to a youth by the K-SADS to the total sum of diagnoses provided by the HCJPD. The average number of diagnoses assigned by the K-SADS was M=5.8 (SD=4.3), while the average number for HCJPD was M=3.4 (SD=1.1). In general, the K-SADS generated more diagnoses of youth but had a larger standard deviation. HCJPD assigned less diagnoses on average; however, they had a smaller standard deviation. Within the current sample, ICC(3,2)=-0.23 (-2.52; -0.57), meaning the two-way mixed effects model was applied with a consistency definition. The ICC results suggest extreme inconsistency in the number of diagnoses assigned for the youth by HCJPD as compared to the K-SADS. Specifically, a negative value is difficult to interpret as an appropriate range for inter-rater reliability would fall within the 0.75 and 0.90 range. This suggests that K-SADS and HCJPD provided very different ratings for the number of diagnoses each youth received.
Table 1 also presents the data on frequency of unspecified diagnoses assigned by K-SADS as compared to HCJPD. Of note, none of the youth used in analyses had an unspecified diagnosis assigned when assessed with the K-SADS. Alternatively, HCJPD assigned up to three unspecified diagnoses (M=0.8, SD=0.9). It was not possible to examine the differences using parametric statistics as the K-SADS did not provide unspecified diagnoses in the matched sample, meaning the variable was a constant (0). Therefore, Cohen’s Kappa did not provide interpretable information.
Please see Figure 2 to examine the prevalence of disorders diagnosed by the K-SADS versus HCJPD. The K-SADS results for diagnosis distribution suggested the largest proportion of diagnoses fell under the substance-related and addictive disorders (39%), followed by DBDs (14%) and anxiety disorders (10%). However, HCJPD assigned an equal proportion of substance related and DBD diagnoses (28%), as well as a high prevalence of neurodevelopmental (23%). The K-SADS provided more variable diagnoses, likely due to the ability to capture internalizing concerns, such as depression or anxiety. However, the K-SADS identified less neurodevelopmental concerns than were identified by the HCJPD.
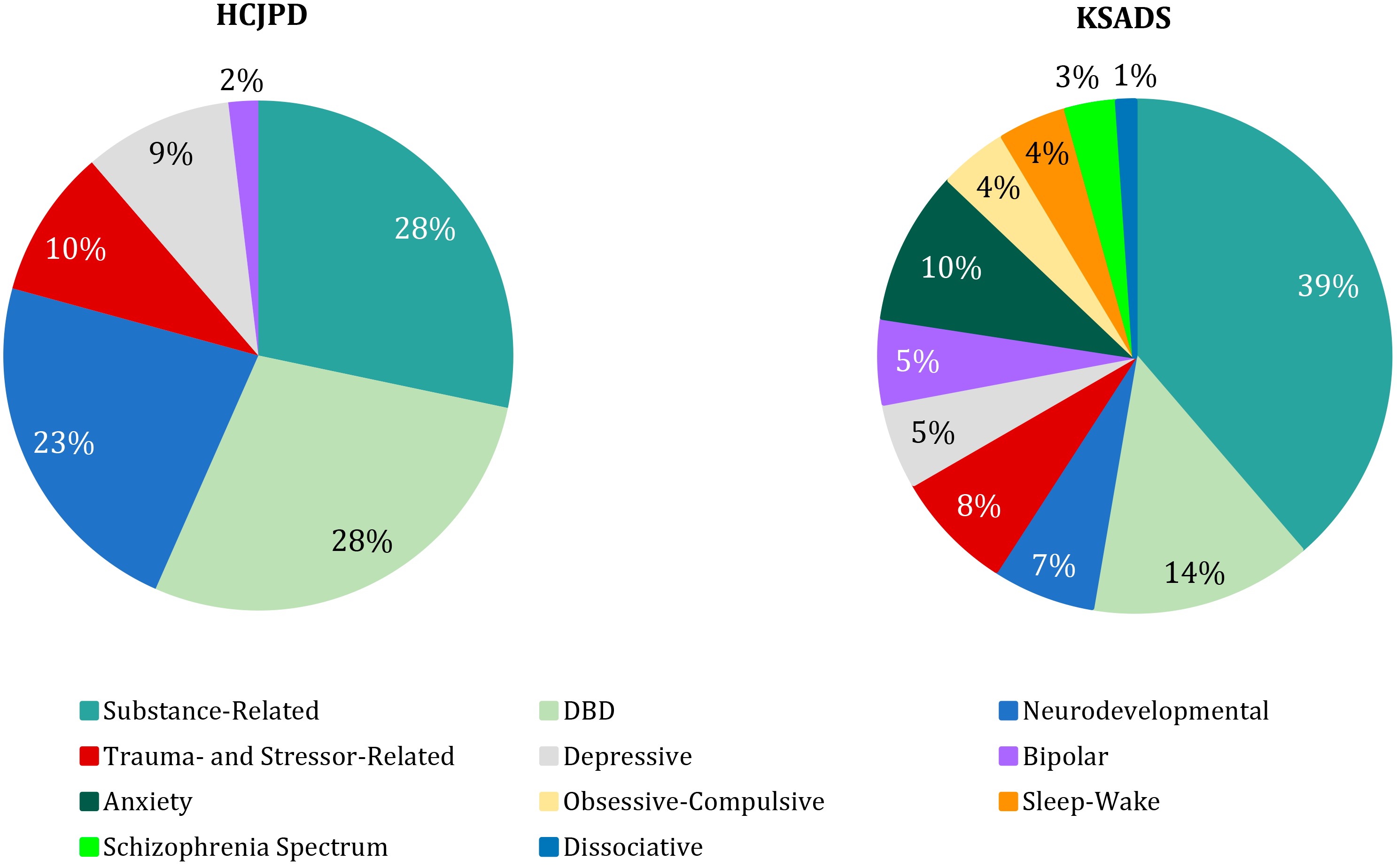
Figure 2. K-SADS Disorder Diagnosis Prevalence for Matched Sample of 16 Youth
Discussion
The discordant (negative) ICC and Cronbach’s alpha results are consistent with the hypothesis that the K-SADS and the HCJPD diagnostic systems differ from each other. In particular, it suggests that the ICC is not interpretable due to the inconsistent assignment of the number of diagnoses between the two sources [22]. The discordant ratings may be due to a series of factors. First, K-SADS follows branching logic, thus evaluating all domains of the DSM-5 [38], while HCJPD may not assess for all possible mental health concerns. Second, K-SADS assesses all youth following the same procedures as it is a semi-structured tool. HCJPD varies its assessment protocol based on a series of factors, including whether a youth is “flagged” during a screener suggesting they need a fuller evaluation. Human bias is introduced with unstructured clinical interviews, which is avoided (at least in part) when using a semi-structured tool, as evidenced by increased interrater reliability [35; 38].
K-SADS provides a fuller evaluation via the screener portion of the assessment, which determines the criteria to further assess to provide the most appropriate diagnosis. It ensures that each diagnostic chapter is assessed, which is not necessarily true of unstructured interviews. The K-SADS total sum of diagnoses also had a larger standard deviation, potentially accurately reflecting the variation in presenting concerns among youth involved with the JJS. Of note, it may be more difficult to establish rapport with a youth while administering a semi-structured tool, which may explain why some youth assessed via the K-SADS did not meet any diagnostic criteria. HCJPD had a diagnosis for every youth, perhaps suggesting they have the opportunity to build a connection with the youth, as a rapport has been found to be an integral piece of therapeutic success [25]. HCJPD provides fewer diagnoses than the K-SADS, which could be due to a number of factors, including limited access to collateral information or limited time with the youth.
Of note, HCJPD assigned a larger number of neurodevelopmental concerns (primarily ADHD). Potentially, the discrepancy was due to HJCPD clinicians having access to medical and/or school records for some of the youth to confirm an ADHD diagnosis, while the K-SADS relied on youth self-report. Interestingly, both HCJPD and the K-SADS identified a large proportion of youth with substance use concerns. It has been noted that both ADHD and SUD concerns have been related to delinquency, in particular, when comorbid with other disorders, internalizing or externalizing [24; 40]. Regarding the unspecified diagnoses, the K-SADS assigned one unspecified diagnosis for the entire sample and none for youth included in the matched sample. HCJPD provided up to three unspecified diagnoses for each youth in the current sample, suggesting limited ability to assess for all criteria necessary for a specific diagnosis. The primary benefit to having diagnoses properly assigned is to provide information to determine the type of intervention and services the youth would benefit from while involved with HCJPD, with some of the available health services including mental health and substance-use specific placements [16]. For particularly at-risk youth, detention facility placements are their only access to health care services, further demonstrating the necessity of addressing youth’s needs while they are involved with the JJS [12].
A strength of the HCJPD clinical interview approach is the ability to indicate “Other Conditions That May Be a Focus of Clinical Attention” for youth, including abuse or family separation. The K-SADS does not provide such data unless a child endorsed abuse or conflict within the PTSD module. While not an official diagnosis, the category of “other conditions” can provide helpful information to understand a youth’s presentation and needs, which may alter the type of intervention or placement the youth receive while involved with the probation department. Research suggests that it is equally important to target criminogenic needs (antisocial peers, poor family dynamics) in addition to mental health needs to limit recidivism and have increased positive outcomes [27; 34].
The risk-need-responsivity (RNR) model, which emphasizes rehabilitation rather than punitive practices, is becoming more widespread in juvenile justice [4]. Appropriate and specific mental health diagnoses (e.g., the needs of the youth) can ensure informed decisions are made regarding placement and treatment (e.g., the response). Of note, HCJPD may be hesitant to assign too many diagnoses due to concerns with negative effects of labeling youth [33; 42]. However, it is important to balance the opportunity to provide the most relevant and beneficial services to juveniles while limiting potentially stigmatizing labels. Given the value of providing appropriate care, in particular, if this is a youth’s first exposure to mental health care services, reliable and valid diagnoses are necessary. Incorporating structured or semi-structured tools into the assessment of juveniles involved with the JJS is a cost-effective way of collecting thorough diagnostic information for youth, including those who may not receive an extensive psychological and academic evaluation otherwise.
Limitations and Future Directions
In the current project, we were able to detect a series of differences between the diagnostic system currently utilized by HCJPD compared to the “gold standard” of mental health assessments. Due to the Covid-19 pandemic and the movement to limit youth’s exposure to the JJS, we were not able to achieve our originally intended sample size due to fewer youth being referred to detention facilities and/or placed on probation [15]. Therefore, the current study has a limited sample, which likely impacted analyses. Specifically, it would be important to examine whether there are diagnostic differences present based on demographics, as has been noted in previous studies [17]. It might be of interest to examine, with a larger sample, whether unspecified diagnoses would be more frequent in the K-SADS sample and whether the distribution of types of diagnoses would differ. The sample may not be representative of all juvenile probation departments, both demographically and regarding diagnostic methodology within the department, as the current sample utilized methods specific to HCJPD. The current distribution of diagnoses may be specific to the current sample and not necessarily generalizable to other counties or probation departments. Overall, the K-SADS captured more variability in mental health concerns in youth involved with HCJPD, including internalizing concerns. However, HCJPD identified a larger proportion of neurodevelopmental concerns (e.g., ADHD) and “Other Conditions That May Be a Focus of Clinical Attention,” which was not captured by the K-SADS.
For future directions, it would be of interest to examine the interaction between the diagnostic approach, interventions provided to the youth, and recidivism rates. If the K-SADS more accurately assigns diagnoses, it could impact the types of services provided to the youth, thus addressing more of their needs, specifically, internalizing or substance use concerns. Future research would benefit from larger and more diverse samples (e.g., gender, race, and age diversity).
References
-
Abrantes A.M., Hoffmann N.G., Anton R. Prevalence of co-occurring disorders among juveniles committed to detention centers. International Journal of Offender Therapy and Comparative Criminology,2005, vol. 49, no. 2, pp. 179‒193. DOI: 10.1177/ 0306624X04269673
-
Althouse R. Standards for psychology services in jails, prisons, correctional facilities, and agencies. Criminal Justice and Behavior, 2000, vol. 27, no. 4, pp. 433‒494. DOI: 10.1177/0093854800027004004
-
Barrett D.E., Katsiyannis A., Zhang D. et al. Delinquency and recidivism: A multicohort, matched-control study of the role of early adverse experiences, mental health problems, and disabilities. Journal of Emotional and Behavioral Disorders, 2014, vol. 22 (1), pp. 3‒15. DOI: 10.1177/1063426612470514
-
Brogan L., Haney-Caron E., NeMoyer A. et al. Applying the risk-needs-responsivity (RNR) model to juvenile justice. Criminal Justice Review, 2015, vol. 40, no. 3, pp. 277‒302. DOI: 10.1177/0734016814567312
-
Couwenbergh C., van den Brink W., Zwart K.et al. Comorbid psychopathology in adolescents and young adults treated for substance use disorders: a review. European Child & Adolescent Psychiatry, 2006, vol. 15, no. 6, pp. 319‒328. DOI: 10.1007/s00787-006-0535-6
-
Dixon A., Howie P., Starling J. Psychopathology in female juvenile offenders. Journal of Child Psychology and Psychiatry, 2004, vol. 45, no. 6, pp. 1150‒1158. DOI: 10.1111/j.1469-7610.2004.00307.x
-
Drerup L.C., Croysdale A., Hoffmann N.G. Patterns of behavioral health conditions among adolescents in a juvenile justice system. Professional Psychology: Research and Practice, 2008, vol. 39, no. 2, pp. 122‒128. DOI: 10.1037/0735-7028.39.2.122
-
Edens J.F., Desforges D.M., Fernandez K. et al. Effects of psychopathy and violence risk testimony on mock juror perceptions of dangerousness in a capital murder trial. Psychology, Crime & Law, 2004, vol. 10, no. 4, pp. 393‒412. DOI: 10.1080/10683160310001629274
-
Fazel S., Doll H., Långström N. Mental disorders among adolescents in juvenile detention and correctional facilities: a systematic review and metaregression analysis of 25 surveys. Journal of the American Academy of Child & Adolescent Psychiatry, 2008, vol. 47,
no. 9, pp. 1010‒1019. DOI: 10.1097/CHI.ObO13e31817eecf3 -
Flamez B., Sheperis C.J. (eds.) Diagnosing and treating children and adolescents: A guide for mental health professionals. Hoboken, New Jersey: John Wiley & Sons, 2015. 544 p.
-
Frances A. (ed.). Essentials of psychiatric diagnosis: Responding to the challenge of DSM-5 (Revised edition). New York, NY: Guilford Press, 2013. 218 p.
-
Golzari M., Hunt S.J., Anoshiravani A. The health status of youth in juvenile detention facilities. Journal of Аdolescent Health, 2006, vol. 38, no. 6, pp. 776‒782. DOI: 10.1016/j.jadohealth.2005.06.008
-
Grisso T., Vincent G., Seagrave D. (eds.) Mental health screening and assessment in juvenile justice. New York, NY: Guilford Press, 2005. 397 p.
-
Haney-Caron E., Brogan L., NeMoyer A. et al. Diagnostic changes to DSM-5: The potential impact on juvenile justice. Journal of the American Academy of Psychiatry and the Law, 2016, vol. 44, no. 4, pp. 457‒469. URL: http://jaapl.org/content/44/4/457 (Accessed: 27.05.2022)
-
Harris County Juvenile Probation Department. 2020 Annual Report. Book 2020 Annual Report. Editor, 2020. 16 p.
-
Harris County Juvenile Probation Department. Health Services. URL: https://hcjpd.harriscountytx.gov/Pages/HealthServices.aspx2022(Accessed: 30.05.2022)
-
Harzke A.J., Baillargeon J., Baillargeon G. et al. Prevalence of psychiatric disorders in the Texas juvenile correctional system. Journal of Correctional Health Care, 2012, vol. 18, no. 2, pp. 143‒157. DOI: 10.1177/1078345811436000
-
Heflinger C.A., Hinshaw S.P. Stigma in child and adolescent mental health services research: understanding professional and institutional stigmatization of youth with mental health problems and their families. Administration and Policy in Mental Health and Mental Health Services Research, 2010, vol. 37, no. 1‒2, pp. 61‒70. DOI: 10.1007/s10488-010-0294-z
-
Kang T., Wood J.M., Eno Louden J. et al. Prevalence of internalizing, externalizing, and psychotic disorders among low-risk juvenile offenders. Psychological Services,2018, vol. 15, no. 1. pp. 78‒86. DOI: 10.1037/ser0000152
-
Kashner T.M., Rush A.J., Surís A. et al. Impact of structured clinical interviews on physicians' practices in community mental health settings. Psychiatric Services, 2003. vol. 54, no. 5, pp. 712‒718. DOI: 10.1176/appi.ps.54.5.712
-
Kaufman J., Birmaher B., Brent D. et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 1997, vol. 36, no. 7, pp. 980‒988. DOI: 10.1097/00004583-199707000-00021
-
Koo T.K., Li M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 2016, vol. 15, no. 2, pp. 155‒163. DOI: 10.1016/j.jcm.2016.02.012
-
Kovalenko J.D., Kulesz P.A., Hein S. et al. The unspecified residual category of the DSM-5: The challenges of a catch-all diagnosis. Current Psychology, 2021, pp. 1‒12. DOI: 10.1007/s12144-021-02077-9
-
Lalayants M., Prince J.D. Delinquency, depression, and substance use disorder among child welfare-involved adolescent females. Child Abuse & Neglect, 2014, vol. 38, no. 4. pp. 797‒807. DOI: 10.1016/j.chiabu.2013.08.008
-
Leach M.J. Rapport: A key to treatment success. Complementary Therapies in Clinical Practice, 2005, vol. 11, no. 4, pp. 262‒265.DOI: 10.1016/j.ctcp.2005.05.005
-
Lüdtke J., In-Albon T., Schmeck K. et al. Nonsuicidal self-injury in adolescents placed in youth welfare and juvenile justice group homes: associations with mental disorders and suicidality. Journal of Abnormal Child Psychology, 2018, vol. 46, no. 2,
pp. 343‒354. DOI: 10.1007/s10802-017-0291-8 -
McCormick S., Peterson-Badali M., Skilling T.A. The role of mental health and specific responsivity in juvenile justice rehabilitation. Law and Human Behavior, 2017, vol. 41, no. 1, pp. 55‒67. DOI: 10.1037/lhb0000228
-
McGraw K.O., Wong S.P. Forming inferences about some intraclass correlation coefficients. Psychological Methods, 1996, vol. 1 (1), 30‒46. DOI: 10.1037/1082-989X.1.1.30
-
Meyer G.J., Finn S.E., Eyde L.D. et al. Psychological testing and psychological assessment: A review of evidence and issues. American Psychologist, 2001, vol. 56, no. 2, pp. 128‒165. DOI:10.1037/0003-066X.56.2.128
-
Murrie D.C., Boccaccini M.T., McCoy W. et al. Diagnostic labeling in juvenile court: How do descriptions of psychopathy and conduct disorder influence judges? Journal of Clinical Child and Adolescent Psychology, 2007, vol. 36, no. 2, pp. 228‒241. DOI: 10.1080/ 15374410701279602
-
Murrie D.C., Cornell D.G., McCoy W.K. Psychopathy, conduct disorder, and stigma: Does diagnostic labeling influence juvenile probation officer recommendations? Law and Human Behavior, 2005, vol. 29, no. 3, pp. 323‒342.DOI: 10.1007/s10979-005-2415-x
-
Rijo D., Brazão N., Barroso R. et al. Mental health problems in male young offenders in custodial versus community based-programs: Implications for juvenile justice interventions. Child and Adolescent Psychiatry and Mental Health, 2016, vol. 10, no. 1, pp. 1‒12. DOI: 10.1186/s13034-016-0131-6
-
Samuel I.A. Utilization of mental health services among African-American male adolescents released from juvenile detention: Examining reasons for within-group disparities in help-seeking behaviors. Child and Adolescent Social Work Journal, 2015, vol. 32, no. 1, pp. 33‒43. DOI: 10.1007/s10560-014-0357-1
-
Schubert C.A., Mulvey E.P., Glasheen C. Influence of mental health and substance use problems and criminogenic risk on outcomes in serious juvenile offenders. Journal of the American Academy of Child & Adolescent Psychiatry, 2011, vol. 50, no. 9, pp. 925‒937. DOI: 10.1016/j.jaac.2011.06.006
-
Segal D.L., Coolidge F.L., O'Riley A. et al. Structured and semistructured interviews. In M. Hersen (ed.), Clinician's Handbook of Adult Behavioral Assessment. Colorado Springs, CO: Elsevier, 2006, pp. 121‒144. DOI:10.1016/B978-012343013-7/50007-0
-
Shufelt J.L., Cocozza J.J. Youth with mental health disorders in the juvenile justice system: Results from a multi-state prevalence study. New York, NY: National Center for Mental Health and Juvenile Justice Delmar, 2006. 6 p. URL: https://www.ojp.gov/ ncjrs/virtual-library/abstracts/youth-mental-health-disorders-juvenile-justice-system-results-multi (Accessed: 27.05.2022)
-
Teplin L.A., Abram K.M., McClelland G.M. et al. Psychiatric disorders in youth at juvenile detention. Archives of General Psychiatry, 2002, vol. 59, no. 12, pp.1133‒1143. DOI: 10.1001/archpsyc.59.12.1133
-
Townsend L., Kobak K., Kearney C. et al. Development of three web-based computerized versions of the Kiddie Schedule for Affective Disorders and Schizophrenia child psychiatric diagnostic interview: preliminary validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 2020, vol. 59, no. 2, pp. 309‒325. DOI: 10.1016/j.jaac.2019.05.009
-
Vacc N.A., Juhnke G.A. The use of structured clinical interviews for assessment in counseling. Journal of Counseling and Development, 1997, vol. 75, no. 6, pp. 470‒480. DOI: 10.1002/j.1556-6676.1997.tb02363.x
-
Von Polier G., Vloet T., Herpertz‐Dahlmann B. ADHD and delinquency —
A developmental perspective. Behavioral Sciences & the Law, 2012, vol. 30, no. 2. pp. 121‒139. DOI: 10.1002/bsl.2005 -
Wasserman G.A., Ko S.J., McReynolds L.S. Assessing the mental health status of youth in juvenile justice settings (Juvenile Justice Bulletin). Office of Juvenile Justice and Delinquency Prevention, 2004. 8p. URL: https://ojjdp.ojp.gov/library/publications/ assessing-mental-health-status-youth-juvenile-justice-settings (Accessed: 27.05.2022)
-
Watson A.C., Kelly B.L., Vidalon T.M. Examining the meaning attached to mental illness and mental health services among justice system-involved youth and their parents. Qualitative Health Research, 2009, vol. 19, no. 8, pp. 1087‒1099. DOI: 10.1177/ 1049732309341202
Information About the Authors
Metrics
Views
Total: 261
Previous month: 21
Current month: 8
Downloads
Total: 94
Previous month: 0
Current month: 1