Introduction
The changes that women experience in the postpartum period concern not only the body, but also the psyche: in particular, personality, emotions, cognitive characteristics [14, etc.], etc. Bodily experience, as a collection of sensations, experiences, and representations related to sensory–empirical and cognitive-mediated reflection of one's body, also changes in the postpartum period. According to the cultural-historical approach, corporeality develops throughout life ([1; 9; 13; 19, etc.]. In adulthood, with sharp changes in corporeality, a person is faced with illness and aging, and a woman - at the birth of a child. The development of corporeality coincides with the development of higher mental functions. In other words, this is the path of lifetime formation, socialization, from the direct process to the indirect, which is carried out with the participation of an adult. That is, when analyzing the development of corporeality, it is necessary to study the social situation of development [Vygotskii, 1984]. It was also revealed that social factors limit female corporeality more than male [8, etc.]. Therefore we assume that the postpartum period is an important stage of psychosomatic development. At the same time, it is worth paying attention to the fact that corporeality was little studied in this period.
Based on the analysis of scientific sources, we identified psychosomatic development factors in this period:
- physiological changes affecting the emergence of new intro- and proprioceptive (from lactation and breastfeeding, restoration of the uterus, etc.) and exteroceptive sensations (related to visual perception of body changes, etc., with perception of sound stimuli from a child, tactile feeling of breast augmentation due to lactation, etc.) [Filippova, 2020].
- the appearance of new formations in the mental sphere, for example, the appearance of the image of a child, more precisely - the concretization of the image that arose at the stage of pregnancy, the appearance of the internal picture of pregnancy, the postpartum period, etc. In this context, mother perceives the child as an integral part of her body [16; 17]: "body boundaries" are re-formed by 4 months after delivery [Pickens, 1982].
- a change in the social role, in particular, the emergence of a maternal role that increases the level of feminization of the body, which is manifested in a change in body shape, gait, etc., the bonding in the mother-child system, for which bodily contact is important, etc. [Filippova, 2020].
Bodily alterations in the maternity patients suggest that her bodily experience has specific features.
When corporeality changes in adulthood, factors that enrich bodily experience are distinguished. In the postpartum period, this is a woman's disease [Vasina, 2011], ideas about the postpartumt period, emotions, personal characteristics [Vasina, 2011a], the social situation of development and existence [Vasina, 2008], etc. It can be a child's disease: for example, some diseases require longer breastfeeding [Fernandez, 1984], and lactation is part of the bodily experience.
In other words, we assume, that the bodily experience of puerperas with sick children is different from that of women with healthy ones.
The purpose of the work - study of the peculiarities of the bodily experience of maternity patients with healthy and sick children.
Organization and methods of research
136 women were studied: 1) 50 women without children, 2) 50 maternity patients with healthy children, 3) 36 maternity patients with sick children.
In order to identify the peculiarities of the bodily experience of the maternity patients, 50 women without children were studied. 56% - with higher education, 44% - with secondary-level education. The selection criteria were: a) age 19 to 30 years (M = 24.62, SD = 2.7); b) absence of a history of pregnancies, serious diseases.
The main testing was carried out at a time of 1.5 months after childbirth.
In order to do this, first, at the age of 3 days after childbirth, women meeting the following criteria were studied: a) 1 pregnancy; b) natural childbirth; c) marriage; d) age from 19 to 30 years. The results are described earlier [Vasina, 2011a]. One of the goals at this time was to establish contact in order to agree on a meeting in 1.5 months. This work was carried out in the maternity hospital of Lyubertsy (head of the department. - N.V. Levkina).
The 1 main group included 50 women at 1.5 months after childbirth. In addition to this, the absence of depression and complications after childbirth and illness in the child was taken into account. 54% - with higher education, 46% - with secondary-level education. Mean age (g): M = 24.84, SD = 2.4.
The second (2) main group consisted of 36 women at 1.5 months postpartum, whose babies developed obstructive bronchitis. Other selection criteria were: a) -d) - as in 1 main group. 52.8% - with higher education, 47.2% - with secondary-level education. Mean age (g): M = 25.17, SD = 2.1. This work was carried out in hospital No. 70 (head department - I.V. Devochkina).
The following methods were used:
1) "Classification of sensations" [Efremova, 1990]. It studied 2 and 3 tasks: selection from descriptors, which, according to women, mean intraceptive sensations, descriptors known from experience with their subsequent free classification. Classification results were processed by TAXON analysis. Before him, the most frequent features were selected (they were distinguished by at least 35% of people: the ratio of creators) [Efremova, 1990]. Such treatment is typical of psychosemancy [10; 15]. Based on distributions of descriptors by women and averaging of these distributions, groups of sensations stood out. Descriptors were ranked by average frequencies of matches with other descriptors of the same group. After that, the frequency of inter-group matches was considered, the groups were structured by taxa layers;
2) "10 sensations";
3) "Scale of sensations in the postpartum period",
4) "Scale of vegetative perception" [Vane, 1998],
5) "Questionnaire for maternity patients",
6) "Body attention questionnaire" (BAQ) by S. Fisher in the adaptation of E.T. Sokolova [Sokolova, 1985]. The methods 2,3,5 were created by the author [Vasina, 2011a] to determine the quantitative and qualitative composition of sensations, and were used in maternity patients.
The programs used were Statistica 6.0 and Jamovi 2.3.21. The folloving methods were used: taxon analysis (psychological method 1), Fisher's exact test (1-6), Mann-Whitney U test (1-3.5), univariate variance analysis with non-parametric Welch correction, post-hoc analysis (Games-Howell test) (4.6).
Results
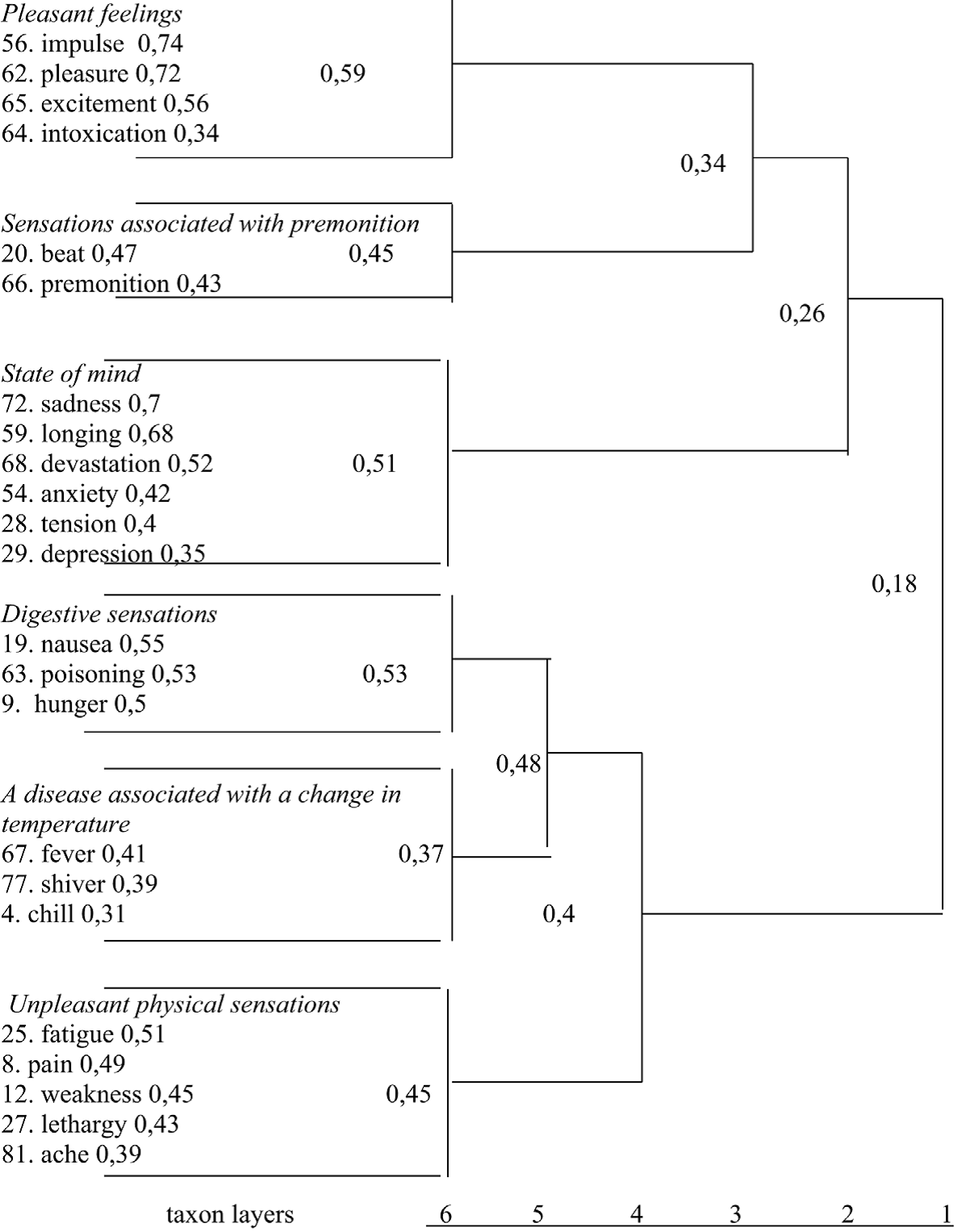
When performing the method "Classification of sensations" on women without children, the TAXON analysis showed (Fig. 1) the formation of 6 layers of taxons. 1 taxon - positive emotional sensations, 2 - sensations of premonition, 3 - negative emotional sensations, 4 - feelings from the gastrointestinal tract, 5 - sensations from illness with fever, 6 - sensations of tone, fatigue and pain. In layer 5, feelings from the gastrointestinal tract and from illness are combined, in layer 4 they
Fig.1. TAXON-analysis of the results of sensation classification (women without children)
merge with unpleasant physical sensations, in 3 - pleasant emotional sensations are combined with sensations of premonition, in layer 2 emotional and physical sensations remain. Therefore, the main categories for sensations are emotional and physical states.
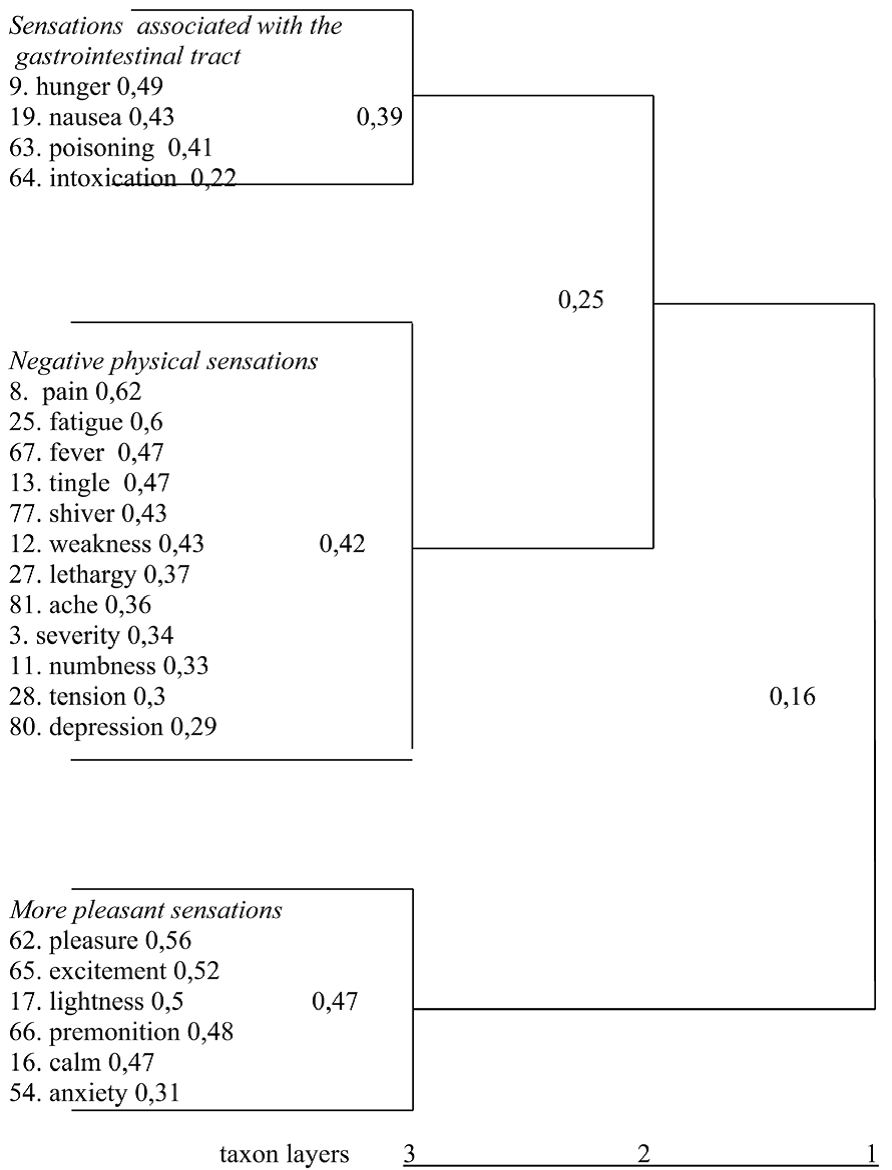
Fig.2. TAXON-analysis of the results of the classification of sensations (maternity women with healthy children)
The familiar dictionary of sensations known from experience in women with healthy children differs from the dictionary of women without children in greater undifferentiation (Fig. 2): 1) emotional and bodily states are not the main categories for describing sensations, the main division is by sign: pleasant and unpleasant, 2) reduced differentiation by the number of groups (in women without children - 6, in maternity patients - 3), 3) emotional and physical sensations - in the same groups, 4) descriptor "anxiety" - in the group "more pleasant sensations": incomplete differentiation by sign. The undifferentiation of the dictionary is associated with the involvement of a huge number of forces, etc., which changes the experience of sensations. Childbirth contributes to an altered state of consciousness [12, etc.], which affects undifferentiality.
In the maternity dictionary, physical sensations prevail over emotional sensations. The volume of the dictionary is similar in maternity patients, and similar to women who have no children. Its internal development by which we mean saturation with verbal forms and verbal nouns, indicating the depth of residence of sensations and concentration on them is also similar with women with children. In maternity patients, the metaphorization of sensations is reduced: in the dictionary - 4 metaphors, in women without children - 9.
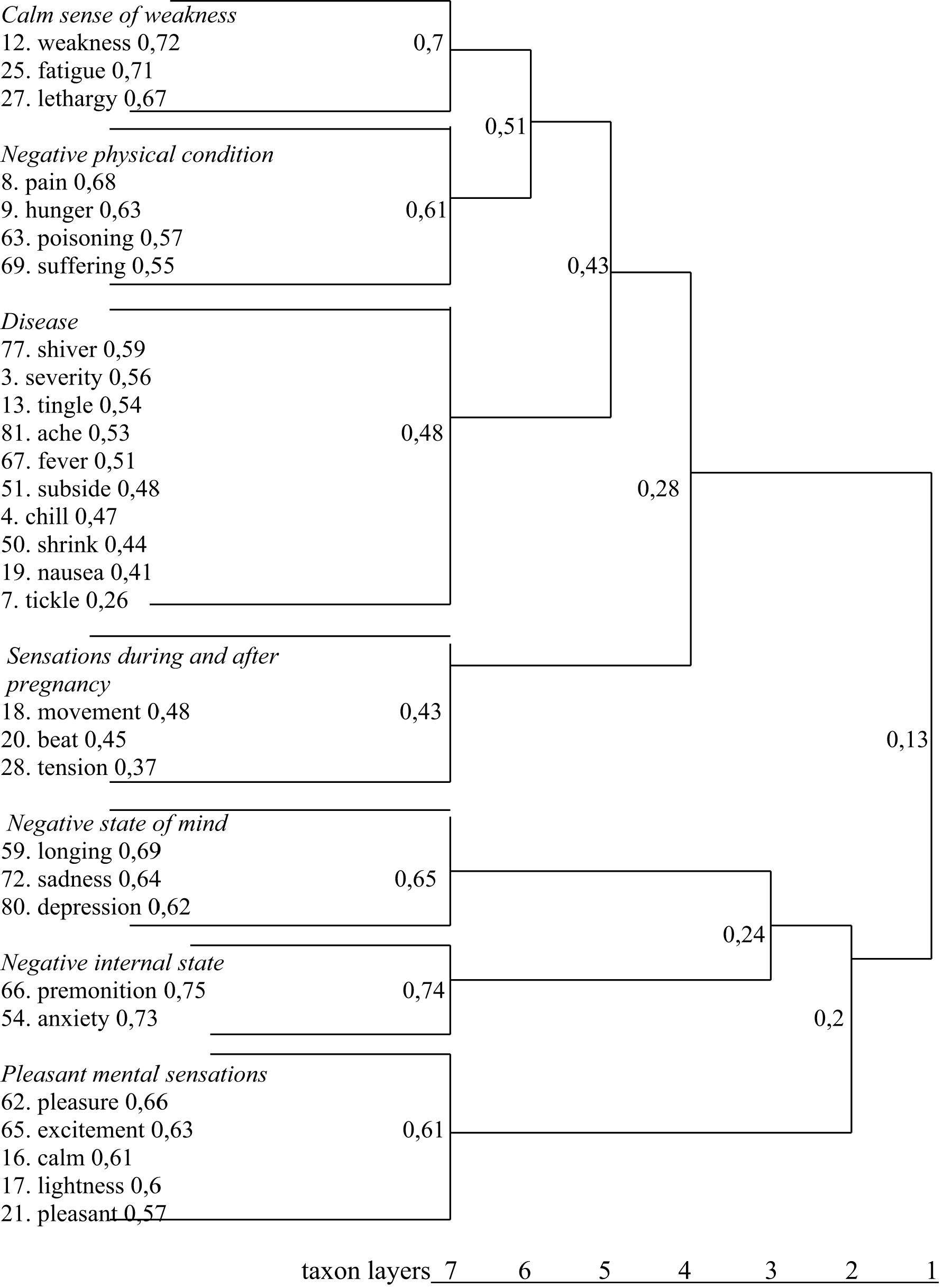
When comparing the results of the method "Classification of sensations" in maternity patients with healthy children and maternity patients with sick children, the TAXON analysis showed (Fig. 3) the formation of 7 layers of taxa with descriptors. 1 taxon - feelings of weakness, 2 - sensations from a negative physical state, 3 - sensations from illness, 4 - sensations during and after pregnancy, 5 - sensations from a negative emotional state, 6 - sensations from a negative internal state, 7 - pleasant emotional sensations. That is, for women with sick children, the usual sensations are less significant. Highlighting groups associated with a negative emotional state suggests that the child's illness causes strong negative emotions experienced at the body level.
The "feeling weak" group means high costs when caring for a child. The dictionary "sensations during and after pregnancy" characterizes the increased importance of communication with a sick child, the desire to consolidate the sensations from it. The basis of "feeling during and after pregnancy" is the only one more often chosen by women with sick children compared to women with healthy ones (33.33% and 6%, respectively, Fisher test φ=3,4403, p < 0.001).
In layer 6, feelings of weakness and sensations from a negative physical state merge, in layer 5 they merge with sensations from a disease, in layer 4 - with sensations during and after pregnancy, in layer 3 sensations from a negative state of mind merge with sensations from a negative internal state, physical and emotional sensations remain in layer 2.
In such a way, unlike maternity patients with healthy children in maternity patients with sick children, the main categories for describing sensations are emotional and physical sensations. The listed is similar in women with sick children and women without children. However, the signs of emotional sensations are not so fully represented, in these 2 categories the emotional sensations are fuller and semantically homogeneous than the signs of physical sensations, which is not the case for maternity patients with healthy children.
The main dividing criterion for emotional states is the sign, as in women without children. The dictionary of negative emotional sensations in women with sick children is differentiated into 2 groups. The fact that they stand out first also speaks of their importance.
The dictionary of women with sick children is more differentiated compared to women with healthy children, i.e. in this it is similar to the dictionary of women without children: 1) in a familiar dictionary of sensations, they have more groups (7 compared to 3), 2) sensations in the 1st queue
Fig. 3. TAXON-analysis of the results of the classification of sensations (maternity women with sick children)
are divided into physical and emotional, 3) physical and emotional sensations - in different groups. More differentiation of sensations means more experience in distinguishing them. A change in the level of wakefulness, which contributes to the undifferentiation of bodily experience after childbirth, is also transformed: the level increases, since a woman needs to respond to the condition of the child.
The average number of sensations in a familiar dictionary in women with healthy children is 22, women with patients - 30: the main increase is due to emotional sensations. In both groups, physical sensations prevail over emotional sensations.
In maternity patients with sick children, there is a higher level of dictionary development: 4 verbs and 12 verbal nouns, in women with healthy ones - 1 and 9. Internal development increases in groups of negative sensations, and the dictionary "sensations during and after pregnancy" consists entirely of verbal nouns.
Metaphorization of sensations is increased in women with sick children: in women with healthy - 4 metaphors, in women with sick - 9, as well as in women without children ("psychologization" of the dictionary).
Comparison of the results of the three samples according to the "Scale of vegetative perception" using a univariate analysis of variance with a non-parametric Welch correction revealed significant differences in the experience of sensations "sometimes weakly" (Welch = 13.7, p < 0.001), "sometimes strongly" (Welch = 31.09, p < 0.001), "often strongly" (Welch = 17.40, p < 0.001), and also in the average number of symptoms (Welch = 29.49, p < 0.001).
Post-hoc analysis (Games-Howell test, Table 1, 2) showed that there is no difference in the intensity and frequency of sensations between maternity women and women who have no children. There is a difference in 26 of 29 sensations (p < 0.05, Fisher test). At the same time, the percentage of maternity patients experiencing each sensation separately is less than the percentage of women without children. This is due to the fact that one of the main sensations is relief from removing the burden of pregnancy: in contrast, ordinary sensations fade.
Table 1
Results on the Scale of vegetative perception (the "*" sign indicates the reliability of differences, p<0.05)
|
Response category (number of selections)
Category of women |
Sometimes weakly |
Sometimes strongly |
Often weakly |
Often strongly |
Average number of symptoms |
|
M (SD) |
M (SD) |
M (SD) |
M (SD) |
M (SD) |
|
|
Women without children |
2,9 (1,4) |
0,9(0,8) |
0,72 (0,6) |
0,24 (0,4) |
4,76 (2,0) |
|
Women with healthy children |
3,76 (2,3) |
0,76 (0,7) |
0,5 (0,6) |
0,38 (0,5) |
5,4 (2,5) |
|
Women with sick children |
5,33 (2,6) |
2,25 (1,0) |
0,44 (0,6) |
1,14 (0,8) |
9,17 (3,0) |
Table 2
The Scale of vegetative perception (post-hock analysis, Games—Howell test)
|
Response category (number of selections)
Category of women |
Sometimes weakly |
Sometimes strongly |
Often weakly |
Often strongly |
Average number of symptoms |
|
Women with healthy children + women with sick children |
MD =-1,57 * р=0,013 |
MD =-1,49 *** р<0,001 |
MD =0,06 р=0,896 |
MD =-0,759*** р<0,001 |
MD =-3,77*** р<0,001 |
|
Women with healthy children+ Women without children |
MD =-0,86 р=0,063 |
MD =0,14 р=0,634 |
MD =0,22 р=0,175 |
MD =-0,14 р=0,288 |
MD =-0,64 р=0,331 |
Note: MD-mean difference; «*» —р<0,05; «***» — р<0,001.
Only one sensation is more often experienced by the delivery women: "blurry vision, specks". It means a violation of the clarity of consciousness, which corresponds to the fact that in this period the state of consciousness changes [12, etc.].
Post-hoc analysis (Games-Howell test, Table 1,2) showed that maternity patients with healthy children differ from those with sick children in the number of sensations experienced "sometimes weakly" (p = 0.013), "sometimes strongly" (p < 0.001), "often strongly" (p < 0.001), and also - the average number of symptoms (p < 0.001). When comparing women with healthy and sick children using the Fisher test, a difference (p < 0.001) was found in 5 sensations: for example, 88% and 66.7% of women, respectively, noted "feeling hot" (φ=2,3926). According to all sensations, the percentage of women with sick children is less than in women with healthy ones: ordinary sensations are unimportant for one group, since sensations from a child are more important.
According to the BAQ method (Table 3,4), the parts of the body that maternity patients think about less often than women without children is neck. The more often they think about the chest, head and torso. Women with sick children, compared to women with healthy ones, are less likely to think about their hands, but more often about their stomach. The belly plays a significant role since it is the space where the child was.
Table 3
BAQ results (the "*" sign indicates the reliability of the differences, p<0.05)
|
Response category Category (average of women rank) |
Chest |
Belly |
Head |
Torso |
Arm |
Back |
Leg |
Neck |
|
M (SD) |
M (SD) |
M (SD) |
M (SD) |
M (SD) |
M (SD) |
M (SD) |
M (SD) |
|
|
Women without children |
5,48 (2,0) |
4,72 (2,4) |
3,5 (2,2) |
4,38 (2,2) |
4,28 (2,0) |
4,28 (2,2) |
3,48 (2,4) |
5,88 (1,9) |
|
Norm, 1.5 months after delivery |
6,38 (1,6) |
4,7 (2,6) |
4,68 (1,9) |
5,70 (1,8) |
4,9 (1,8) |
4,5 (2,1) |
3,08 (1,5) |
2,14 (2,0) |
|
Women with sick children |
6,67 (1,5) |
6,97 (1,1) |
4,47 (1,2) |
5,61 (1,6) |
1,58 (0,8) |
5,22 (1,3) |
3,64 (1,6) |
1,86 (1,0) |
Table 4
BAQ (post-hock analysis, Games—Howell test)
|
Response category (average Category rank) of women |
Chest |
Belly |
Head |
Torso |
Arm |
Back |
Leg |
Neck |
|
Norm, 1.5 months after childbirth + women with sick children |
MD = –0,287 р = 0,670 |
MD = –2,27 *** р<0,001 |
MD = 0,208 р = 0,811 |
MD = 0,089 Р = 0,967 |
MD = 3,32 *** р<0,001 |
MD = –0,722 р = 0,123 |
MD = – 0,0559 р = 0,123 |
MD = 0,279 р = 0,678 |
|
Norm, 1.5 months after delivery + Women without children |
MD = –0,9* р = 0,045 |
MD = 0,02 р = 0,999 |
MD = –1,18 * р = 0,012 |
MD = 1,32** р = 0,003 |
MD = –0,62 р = 0,244 |
MD = –0,22 р = 0,865 |
MD = 0,4 р = 0,577 |
MD = 3,74* *** р<0,001 |
Note: MD-mean difference; «*» —р<0,05; «***» — р<0,001.
According to the "10 sensations" method, the following number of maternity patients of the "normal" group calls the following: feeling from the absence of the abdomen - 64%, fatigue - 56%, feeling from the uterus - 44%, lactation - 36%, etc. Women with sick children call: relief - 44.44%, pleasure from touch - 38.89% (among women with healthy children it is noted only in 2%, φ=4,8631, p < 0.001), a surge of strength - 33%, "joy from admiration of the child felt by the body", etc. - 33.33% (among women with healthy children they it is called only among the 2%, φ=4,3279, p < 0.001), etc. The average number of sensations in the "normal" group in the "10 sensations" method is 3,63±1,8 sensations, in maternity patients with sick children - 3,46±1,9 (the difference is insignificant), typical sensations:
|
Women with healthy children |
Women with sick children |
|
1) relief 2) fatigue 3) sensations from uterine contraction 4) sensations from the lactation |
1) relief 2) the pleasure of touch 3) a surge of strength / joy felt by the body |
According to the Scale of sensations in the postpartum period (Table 5) women with healthy children compared to women with sick children experience fewer "sometimes strongly" sensations.
Table 5
Results on the Scale of sensations in the postpartum period (the "*" sign indicates the reliability of the differences, p<0.05)
|
Response category (number of selections)
Category of women |
Sometimes weakly |
Sometimes strongly |
Often weakly |
Often strongly |
Average number of symptoms |
|
M (SD) / M (SD) |
M (SD) / M (SD) |
M (SD) / M (SD) |
M (SD) / M (SD) |
M (SD) / M (SD) |
|
|
Women with healthy children / women with sick children
|
6,3 (1,7) / 5,28 (1,5) |
0,86 (0,4) / 3,11 (1,1) * |
1,86 (1,4) / 1,11 (0,4) |
1,3 (,5) 1,11/(0,5) |
10,32 (13,8) / 10,61 (2,9) |
When comparing maternity patients with healthy children and maternity patients with patients according to the Fisher test, there is a difference (p < 0.001) in 7 sensations: for example, 40% and 5.6% of women noted "weakness", respectively (φ=4,8631). According to most feelings, the percentage of women with sick children turns out to be less than in women with healthy ones: feelings of weakness, etc., are less important for maternity patients with sick children, the concentration on feelings from the child is 1 plan.
In the Maternity Questionnaire, women with sick children more often than women in the normal group indicated that there were no new feelings after childbirth. However, touching the child was noted more often (33.33% and 2% of women, respectively, φ=4,8631, p < 0.001) and emotions experienced at the body level. Feeding, as a new sensation, was more often called by women with sick children (1 place), breast condition was called as the first less often.
In other words, the bodily experience of childbirth differs from that of women without children as follows: 1) the same volume of the dictionary of descriptors known from experience with a change in content: increase of general tone sensations, less internal development of content of group of pleasant sensations, reduction of number of sensations from negative emotional state, 2) undifferentiation of physical and emotional sensations, physical sensations by systems and organs, 3) the main division of sensations is by sign, but it also has an incomplete undifferentiation, 4) reduced metaphorization, 5) predominance of physical sensations over emotional sensations, 6) similar internal development, 7) slightly increased frequency of sensation occurrence, 8) one of the main sensations is physical relief, 10) the presence of sensations associated with impaired clarity of consciousness, 11) less spatial diversity of sensations.
In maternity patients with sick children, compared with maternity patients with healthy children, the bodily experience differs in the following:
1) scope: a) expanding the composition of descriptors known from experience by expanding negative and positive emotional sensations, sensations during and after pregnancy and negative physical sensations, but not specific to the postpartum period or not locally painful; and sensations associated with a violation of general tone and emotional tension, experienced at the body level, characterized by increased frequency and intensity, b) the number of physical sensations prevails over the number of emotional ones;
2) content: a) dictionaries of sensations are more metaphorized, b) concentration on sensations in the abdomen is more frequent, in the hands is more rare, c) a dictionary of sensations known from experience in maternity patients with sick children looks more like a dictionary of women without children compared to maternity patients with healthy children, d) a dictionary of familiar sensations is more developed, especially - a dictionary of "sensations during and after pregnancy", "negative physical condition", "illness", the latter group has developed a part related to emotional tension experienced at body level, e) bodily experience is characterized by the involvement of the emotional sphere in the bodily, f) the state of the breast acts less often as a new sensation, sensations from touching the child, as well as emotions experienced at the body level act as new sensations of the postpartum period; these women are characterized by a concentration on touch,
3) structure: a) the dictionary "sensations during and after pregnancy" appears, b) "sensations during pregnancy" is more often chosen as the basis for classifying familiar sensations, c) the dictionary of sensations is characterized by increased differentiation.
Discussion
Among the differences in the bodily experience of women with sick children, the concentration on the sensations of the child and their inclusion by women in their bodily experience are especially important for practical use.
Despite the fact that the mother and the newborn exist in unity (on the part of the child, L. Vygotsky denotes this consciousness of mental community as the consciousness of "pra-we" [Vygotskii, 1984], E. Erickson, D. Vinnikot, M. Mahler, D. Stern and others, consider mother and child as part of a single dyadic system, etc.) [cite. 14 et al.], the maternity patient does not attribute the feeling from the child to her bodily experience. The increased connection with the child in maternity patients with sick children is present in the form of a designation of sensations from the child in her bodily experience.
Back at the turn of the 20th-21st century, the principle of sterility prevailed in medical institutions, which implies restricting the admission of parents to the hospital to a child. Now the understanding that the stay of the child with the mother creates a favorable emotional atmosphere for the recovery of the child goes to 1 plan. Changing the bodily experience of maternity patients with sick children by incorporating child-related sensations into it is a factor further showing the importance of mother-child hospital stays together. This can be explained by the fact that in addition to the emotional discomfort of the child, arising in the event of their separation and affecting the recovery of the child, his emotional state is influenced by the state of the mother. The emotional state of the mother worsens, which is associated not only with experiences for the health of the child, but also with the inclusion of sensations from the child in her bodily experience, i.e. the feeling of the temporary loss of a part of herself.
Today, the idea of the importance of staying together is increasingly resonating, but due to changes in the epidemiological situation, the principle of sterility has begun to take up more space. We hope this work will be one of the factors that do not allow the principle of sterility to outweigh the principle of the importance of the emotional connection between mother and child.
Conclusion
- The postpartum period is one of the stages of the psychosomatic development of a woman with changes in the content, volume and categorical structure of bodily experience.
- The normal or complicated course of the postpartum period affects the specifics of bodily experience.
2.1 The bodily experience of maternity patients with healthy children is characterized by richness, internal development, predominance of the number of physical descriptors over emotional ones, incomplete differentiation, change in the main criterion for the classification of sensations (division by sign), low metaphorization.
2.2 The bodily experience of maternity patients with sick children is manifested in an increased concentration on the sensations of the child, experiencing emotional tension and anxiety at the body level, a developed system of interaction with bodily sensations, and higher internal development.
- The results increase the importance of mother-child postpartum co-stay when placing a child in a hospital.
A comparative analysis of the bodily experience of women without children and the bodily experience of maternity patients made it possible to distinguish the features of the bodily experience of maternity patients. Comparison of the bodily experience of maternity patients with healthy and sick children revealed the features of maternity patients with sick children. One of the important characteristics of the bodily experience of maternity patients with sick children is the concentration on the sensations of the child and their inclusion by women in their bodily experience.
The results increase the significance of mother-child postpartum co-stay when the child is admitted to hospital. This adds the factor of the emotional well-being of the mother associated with both the experiences of the child's health and the inclusion of the sensations of the child in her bodily experience to the factor of the importance of the emotional comfort of the child when staying together with the mother in the hospital. In such a way, it follows from the work that the emotional state of the maternity patient with a sick child, which is considered very important for the child, can be deteriorated due to a separate stay, since the mother can feel parting with the child as a temporary loss of part of herself.
The work can be continued as part of the study of other categories of maternity patients, other aspects of the bodily experience of maternity patients with sick children, etc.