INTRODUCTION
Following the growing global focus on deinstitutionalization in the past 50 years, accessible community mental health services were highlighted as a commitment in the European Mental Health Action Plan 2013–2020, with the goal of improving the well-being of patients and families.1 Georgia has made commendable efforts to reform mental health care in recent years, motivated by the growing need for affordable and efficient community mental healthcare.2
Georgia’s mental health care system is managed by the Ministry of Internally Displaced Persons from the Occupied Territories, Labor, Health, and Social Affairs of Georgia (IDPLHSA), which oversees health and social welfare. The ministry supports and coordinates the preparation of the legislation, strategies, action plans, and state programmes that should be adopted by the Government and the Parliament.
The “Concept on Mental Health Care”3 and the two strategic plans for 2014–2020 and 2021–2031, which have been developed and approved by the Government,4 aimed to develop comprehensive evidence-based, culturally appropriate, and human rights-oriented mental health and social care services. The Georgian mental health state programme, which has been functioning since 1995, became the subject of significant amendments in 2018. The budget has been increased significantly and more than half of the funding has been allocated to developing community services, such as community-based ambulatories and mobile teams.
Along with an increased budget (of 8,000,000 GEL), new standards for community-based services have been introduced and incorporated into the mental health state programme. The number and location of community services and the funding methodology have been changed and defined according to the populations of the catchment areas. These changes contributed to achieving the indicator set by the mental health strategic document and the corresponding action plan for 2015–2020. The strategic document specified that by 2020 the ratio between community and institutional services in Georgia should have been 50:50. Introducing the standard of a qualitatively new type of outpatient service changed the ratio established in 2017 (7:75) to the ratio 48:52 in 2021.
The community mental health care services in Georgia include:5
Community ambulatories — specialized secondary level services, which provide care for persons with mental disorders within the area of their residence. Outpatient services are based on the biopsychosocial model and a multidisciplinary approach. Each centre serves a population of 70,000 to 100,000 inhabitants and has a staff of one psychiatrist, 1.5 nurses, and 1.5 psychologists.
Community mobile teams — intensive care for people with severe mental disorders who are frequently hospitalized or stay in hospital for a long time.
The multidisciplinary team consists of three to four staff members, including a psychiatrist, nurse, social worker, and/or psychologist. The team develops an individual care plan for each patient based on the recovery model and provides home care.
Currently, 33 mobile teams are operating countrywide, but the number and composition of the teams need further development.
Mental health crisis intervention centres for adults (aged 16–65 years) — a specialized service which serves individuals living in a particular catchment area (one team per 150,000 inhabitants) with the goal of reducing psychiatric hospitalizations. The teams consist of one team leader, one psychiatrist, one psychologist and one social worker per 20 cases. The team serves people with acute mental health problems. These services can be provided at home (with two daily visits possible), or a person can be transferred to the crisis intervention centre. As the crisis resolves, the person must be referred to less intensive mental health services.
Residential/home care for persons with mental disorders — a specialized mental health service that offers supported housing and appropriate care to ensure the social adaptation and integration of the person with a mental disorder, as well as the maintenance/development of their independent living skills. The assisted living facilities offer different levels of support corresponding to the diverse needs of people with mental disorders. They provide a homelike setting, organized on a recovery model and different levels of therapeutic intervention.
The distribution of the services across the regions is shown in the figure (Figure 1).6
THE AIM AND METHODS OF THE STUDY
The study aimed to investigate the quality of the care provided by the community services, such as mental health ambulatories and mobile teams, and to develop recommendations for the further improvement of the standards of care based on the results.
As a result, we monitored the mental health ambulatories in all major cities and regional centres of the country (in total, 16 ambulatories) and the mobile teams with at least two years of experience (in total, 14 mobile teams).
The quality of care and standards of services have been studied using the following tools:
- The WHO QualityRights tool kit for assessing and improving quality and human rights in mental health and social care facilities.7
- The service monitoring tools for ambulatories (Appendix 1).
- The service monitoring tools for mobile teams (Appendix 2).
The service monitoring tools are the standardized instruments, which have been developed by the working group of experts approved by the Ministry of the Health of Georgia (number of document №01-109/ო, 27.05.2017). Independent monitoring groups made up of three to four members visited the services on the spot. The information was obtained from the following sources:
The service documentation — employment contracts, internal orders and regulations, medical records, lists of the available medications, etc.
Structural interview — the standardized questionnaire based on the WHO QualityRights tool kit and monitoring tools have been used to interview the multidisciplinary team members — psychiatrists, nurses, psychologists, social workers, services users, and caregivers.
The aim and procedures of the study were clearly described to the participants. All participants signed the informed consent.
RESULTS AND DISCUSSION
The increased budget and introduction of new standards for ambulatories and the development of mobile teams organized in all country regions have significantly increased the capacity for mental health care. The medication supply of the community services has substantially improved. The implementation of the recovery model and multidisciplinary teamwork has stimulated the development of biopsychosocial treatment approaches. More mental health professionals, e.g., psychiatric nurses, psychologists and social workers, have been trained and employed.
Table 1. Number of Visits per Three Months
|
Ambulatory N |
Number of registered patients |
% of population |
Number of visits |
Number of home visits |
Total visits |
Number of possible visits/per three months |
|
1 |
10040 |
2,9 |
776 |
89 |
865 |
0 |
|
2 |
3162 |
0,7 |
1105 |
6 |
1111 |
1 |
|
3 |
2576 |
1,4 |
570 |
31 |
601 |
1 |
|
4 |
4165 |
1,2 |
994 |
2 |
996 |
1 |
|
5 |
799 |
0,8 |
180 |
12 |
192 |
1 |
|
6 |
4568 |
2,0 |
810 |
10 |
820 |
1 |
|
7 |
5810 |
4,1 |
775,5 |
4,5 |
780 |
0 |
|
8 |
301 |
0,5 |
160 |
6 |
166 |
2 |
|
9 |
1034 |
1,4 |
246 |
2 |
248 |
1 |
|
10 |
763 |
0,5 |
438 |
39 |
477 |
2 |
|
11 |
7500 |
1,4 |
1940 |
4 |
1944 |
1 |
|
12 |
3456 |
2,1 |
820 |
10 |
830 |
1 |
|
13 |
14829 |
5,9 |
1100 |
3 |
1103 |
0 |
|
14 |
738 |
0,8 |
305 |
4 |
309 |
1 |
In parallel to these remarkable achievements, the following challenges and barriers have been identified:
The official number of patients registered with the community services exceeds the real number of service users. This statistical discrepancy distorts the actual need for mental health care services. In the table (Table 1), we can see that if the ambulatory serves all registered patients, then according to the official number of visits, this number of patients are not able to visit the ambulatory at least once per three months. There is an imbalance between biological and psychosocial care.
Рисунок 1. Картография предоставления услуг в области психического здоровья в Грузии.
The services predominantly offer biological treatment. The patients are generally seen by psychiatrists and receive psychopharmacological treatment. Hence, the psychiatrists are overloaded; sometimes, the psychiatrists have 15–20 or more patients per day while their appointment hours are five hours per day, and the average appointment time is approximately 20–25 min. Thus, the maximum number of patients per day per psychiatrist should not exceed 15–18 patients (Table 2).
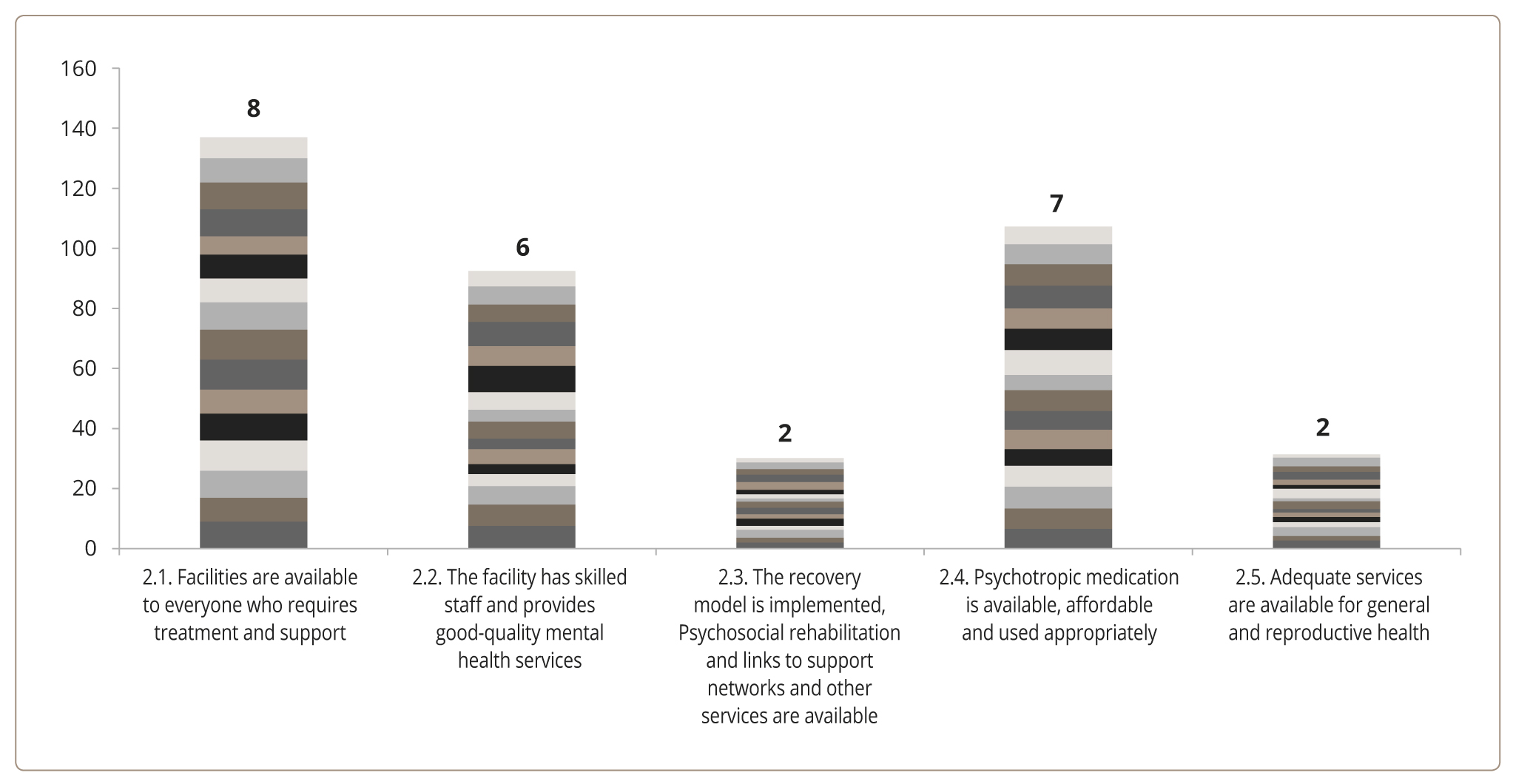
According to the standards for community mental health ambulatories and mobile teams in Georgia, there are enough psychiatrists and psychologists in most community services, but still a shortage of qualified nurses and social workers. The average points for the WHO QualityRights tool kit standard 2.2.8 — “The facility has skilled staff and provides good-quality mental health services” were six points out of 10 (Figure 2).
The score for the WHO QualityRights tool kit standard 2.3. “Treatment, psychosocial rehabilitation, and links to support networks and other services are elements of a service user-driven recovery plan and contribute to a service user’s ability to live independently in the community” varied from very poor to poor (≈ two out of 10 points). Hence, the recovery model for care and multidisciplinary teamwork is not implemented properly, and the resources of other mental health professionals are not used accordingly (Figure 2).
Table 2. The Average Psychiatrists’ Workload in Outpatient Services
|
N of Ambulatory |
Number of visits in ambulatories per month |
Number of home visits per month |
Number of Psychiatrists |
Number of Daily visits |
|
5 |
305 |
14 |
2 |
8,9 |
|
1 |
360 |
16 |
2 |
10,4 |
|
8 |
180 |
12 |
1 |
10,7 |
|
9 |
775,5 |
45 |
4 |
11,4 |
|
2 |
1570 |
31 |
7 |
12,7 |
|
11 |
438 |
32 |
2 |
13,1 |
|
14 |
810 |
10 |
3 |
15,2 |
|
15 |
861 |
2 |
3 |
16,0 |
|
4 |
1776 |
68 |
6 |
17,1 |
|
3 |
3100 |
89 |
10 |
17,7 |
|
6 |
3940 |
20 |
12 |
18,3 |
|
7 |
2105 |
6 |
6 |
19,5 |
|
10 |
1420 |
10 |
4 |
19,9 |
|
13 |
1494 |
14 |
4 |
20,9 |
|
12 |
446 |
2 |
1 |
24,9 |
There are significant differences in fund distributions for medications, administrative, and other expenses across the services, which cannot be explained by the number of patients or the workload of mental health professionals and mainly depend on the subjective interpretation of need by the owners or directors of the services (Table 3).
Table 3. Fund Distribution in Outpatient Services (in GEL)
|
Index |
Max |
Min |
P-value |
|
Index of Medications (% from the total budget) |
66 |
32 |
0,01 |
|
Index of salary for a Psychiatrist |
1900 |
550 |
0,00 |
|
Index of salary for a nurse |
1200 |
300 |
0,00 |
|
Index of salary for a psychologist |
1500 |
400 |
0,00 |
|
Index of salary for a social worker |
1000 |
125 |
0,01 |
The results of the WHO QualityRights tool kit interviewing tools have revealed that most of the community mental health ambulatories have good infrastructure, satisfying physical conditions, and a comfortable environment, but lack sufficient space for psychosocial activities. The services are available to everyone who requires treatment and support (≈ nine points out of 10).
The psychiatrists are qualified to provide psychopharmacological treatment. Psychotropic medication is available, affordable, and generally used appropriately. However, the successful implementation of a recovery-oriented model and psychosocial treatment requires additional effort. The reproductive and somatic health of the patients lacks sufficient attention. The patients with serious mental disorders who are on long-term antipsychotic treatment have limited access to necessary laboratory tests and instrumental exams (Figure 2).
Рисунок 2. Данные набора инструментов ВОЗ QualityRights Группа 2. Право на наивысший достижимый уровень физического и психического здоровья (статья 25 Конвенции о правах инвалидов (КПИ).
Standard 2.1. Facilities are available to everyone who requires treatment and support — eight points out of 10.
Standard 2.2. The facility has skilled staff and provides good quality mental health services — six points out of 10.
Standard 2.3. The recovery model is implemented. Psychosocial rehabilitation and links to support networks and other services are available — two points out of 10.
Standard 2.4. Psychotropic medication is available, affordable, and used appropriately — seven points out of 10.
Standard 2.5. Adequate services are available for somatic and reproductive health — two points out of 10.
There is a significant deficiency of certified social workers, especially in the regions. Therefore, in most community services, the personnel working as social workers do not have specialized education. A lack of qualified social workers and a shortage of social programmes in the community prevent resocialization and the provision of support for independent living.
In mobile teams, the numbers, qualifications, and skills of mental health professionals (e.g., the numbers of nurses, psychologists, and social workers) differ across the services, which considerably influences the quality of care.
The mobile team assessment scale, which rates the structure and composition of human resources, the nature of services, and organizational boundaries, showed an unequal distribution of resources and service provision. Only half of the mobile teams with two or more years of experience showed desirable results and fully or nearly fully could implement the standards of care and receive <85 out of a total 100 points (Table 4).
Table 4. The Mental Health Mobile Team Care Assessment Scale
|
Mobile Team N |
Human resources (35) |
Organizational boundaries (40) |
Nature of services (25) |
Total (100) |
|
1 |
32 |
37 |
24 |
93 |
|
2 |
34 |
40 |
19 |
93 |
|
3 |
31 |
37 |
22 |
90 |
|
4 |
35 |
34 |
19 |
88 |
|
5 |
28 |
37 |
22 |
87 |
|
6 |
27 |
37 |
23 |
87 |
|
7 |
29 |
37 |
20 |
86 |
|
8 |
24 |
38 |
21 |
83 |
|
9 |
28 |
35 |
20 |
83 |
|
10 |
30 |
30 |
17 |
77 |
|
11 |
27 |
29 |
20 |
76 |
|
12 |
23 |
35 |
18 |
76 |
|
13 |
20 |
29 |
23 |
72 |
|
14 |
19 |
29 |
14 |
62 |
The wages of mental health professionals vary and are based on the subjective decision of the administration rather than on objective criteria (qualifications, working hours, workload, etc.).
Some mobile teams share their offices with other mental health services, mainly with ambulatories, which increases the risk of access to patients’ personal information and raises confidentiality issues.
CONCLUSION
Based on the results, the following recommendations have been proposed to the authorities and stakeholders:
The surveillance system, staffing, and care standards should be developed according to the methodology of the WHO Mental Health Policy and Service Guidance Packages “Human resources and training in mental health”9 and “Planning and budgeting to deliver services for mental health.”10
The assertive involvement of all mental health professionals (e.g., psychiatric nurses, psychologists, social workers, etc.) will enhance the accessibility and quality of care. The number of visits and consultations could be increased, and the service users could receive comprehensive biopsychosocial treatment.
The successful implementation of the recovery model requires continuing excellence in professional education. Training in human rights issues and recovery treatment should be routinely offered to psychiatrists and other mental health professionals. The regular monitoring and supervision of services are essential predictors for the further improvement of service delivery.
The introduction of the objective parameters for fund distribution warrants an equitable and fair funding system.
The strong liaison and developed referral system between mental and general health services will improve the quality of somatic and reproductive care and overall outcomes for people with mental and physical health problems.