INTRODUCTION
Bulgaria has around 7 million inhabitants that include a small Turk (8.4%) and Roma (4.4%) populations. Residents in cities (78%) predominate over those in rural areas (22%) in a territory of over 110,879 km2. Bulgaria joined the European Union (EU) in 2007 and ranks 71st in the world in per capita GDP (gross domestic product). The Health Act was introduced in 2005 for the first time, although some efforts in that direction had been made prior.
The dispensary health care system during state socialism1 in Bulgaria covered multiple aspects: “continuous, close monitoring of patients and the study of their (and their families’) needs and lifestyles”, “efforts towards the fullest possible satisfaction of patients’ needs in specialized psychiatric treatment, social support, employment and rehabilitation, legal aid”, expert and prophylactic care aimed at creating a healthier environment, health education, as well as early detection of illness and relapse. The entry point into the system was via so-called dispensary registration. Dispensarization, in its most basic form, was provided for by the Public Health Act of 1973, while the particular ordinance concerning the dispensarization of persons with mental health conditions was issued as late as 1987 [1].
The mental health infrastructure in Bulgaria, by common consensus among the Ministry of Health (MH), the Bulgarian Psychiatric Association, medical, nursing, and other staff, patients, and families, is wanting, and there is a pressing need for reform. Attempts at such reform have stalled so far due to the complexity of arranging funding and a lack of consensus among the stakeholders [2].
HISTORICAL ACCOUNT
Mental health care was never a priority in the health system of Bulgaria: there were very few treatment facilities for the mentally ill before the coup d’état of September 9, 1944. The new regime also failed to recognize it as a priority; mental health care was conspicuously absent in the first program of the Fatherland Front, the communist-dominated coalition that came to power after the coup. From the early 1950s onwards, the new and major undertaking became to develop an outpatient system which was epitomized by the dispensary approach. As the embodiment of social psychiatry with its “prophylactic orientation”, the dispensarization project had to cover many aspects and fulfill the high hopes of the Bulgarian psychiatric community for “bringing psychiatry closer to society” [3].
Dispensarization was meant to be an expression of “the prophylactic trend in socialist healthcare”, to quote Petar Kolarov, which was presented as the latter’s basic principle [4]. Complete dispensarization sought to create — in the words of Todor Zhivkov — “such an environment and responsibility that every citizen in our country, from cradle to the grave, would have a personal file and be monitored and cared for”. Consistently with this attention to creating a healthier environment, including a healthier social environment, the dispensary approach was conceptualized as the embodiment of social psychiatry. The latter was usually presented as follows: social psychiatry means “bringing psychiatric care as close to the social community as possible”. Precisely social psychiatry had “raised the authority of psychiatry and brought it up to par with a number of leading medical disciplines” [5]. This was in keeping with the Soviet model of dispensarization, which was adopted by Bulgarian psychiatry.
The dispensary system in the period of state socialism in Bulgaria included multiple activities: “continuous, close monitoring of patients and studying their (and their families’) needs and lifestyles”, “fullest possible satisfaction of patients’ needs in specialized psychiatric treatment, social support, employment and rehabilitation, legal aid”, expert and prophylactic activities aimed at creating a healthier environment, health education, early detection of the disease, and relapse [6]. Entry into this system was via so-called dispensary registration. Dispensarization — in its most basic form — was enshrined in the Public Health Act of 1973, while the specific legal framework concerning the dispensarization of persons with mental health conditions was issued as late as 1987 [7].
Both before and immediately after 1917, the view that better mental health was the natural result of improved social conditions was particularly popular among the Russian psychiatric community. This model received further ideological justification after the October Revolution of 1917, and this put a trump card in the hands of psychiatrists who wanted to reorganize the system in a prophylactic spirit. The most outstanding among them was Lev Rozenshtein, who became the “father” of the dispensary model — directed and financed by the state — in the Soviet Union. His idea of “neuropsychiatric dispensaries” originated specifically in his interest in alcoholism, but he was in fact the first to turn the dispensary into a form of “consolidated institutional care for alcoholic and nervously ill patients” [8].
CURRENT STATUS
The main aspects of the current situation are characterized by a deep fragmentation of outpatient mental health care, which is not properly integrated with other services in health care delivery, or with other tangential aspects of the public sector such as social services, education, and justice, among others. Legitimate patient organizations are not adequately represented on the level of health policy in psychiatry. These shortcomings have to do with the lack of a holistic approach to psychiatric care.
Data from an epidemiological study conducted in 2011 shows that all respondents with a common mental disorder in the 12-month period that had preceded the interview had received help (20.69%). For 19.7% of them, the help assumed the form of medication: 16.85% saw a general practitioner, while 5.58% were examined by a psychiatrist. Interestingly, 3.75% of those without a medical condition aligned with the criteria of the study also sought medical care for related mental health problems. People with panic disorder — 59.34%, followed by those with dysthymia — 43.44%, and those with a depressive episode — 32.33%, and those with post-traumatic stress disorder — 31.74%, received medical treatment most frequently. Two to three times less frequently people with generalized anxiety (17.73%) and phobias (14.32%) received treatment. People with substance use disorders in the 12 months preceding the interview received care in only 3.95% of the cases (2.35% by a psychiatrist). People with panic disorder saw a psychiatrist most often (20.47%), followed by those with generalized anxiety disorder (11.78%) and recurrent depressive disorder (11.52%). Non-medical services came into play relatively infrequently, at 0.99%. Most of the people with post-traumatic stress disorder (PTSD) represented 7.44%. A telling fact about recognition of this diagnosis in Bulgaria is that of the same group of people only 3.75% received qualified psychiatric care [9]. A second epidemiological study was conducted in Bulgaria, EPIBUL-2, in 2017 [10], but the results have not been published.
HUMAN RESOURCES
There is a shortage of medical specialists in all fields throughout Bulgaria. Psychiatry is among the most affected fields in terms of staff insufficiency. There is also a problem with several lines of funding for the various psychiatric structures, which leads to an uneven distribution of doctors in them.
In the field of mental health in Bulgaria, medical doctors can specialize in three areas: psychiatry, forensic psychiatry, and child psychiatry. These are independent medical fields, which means that it is not necessary to first acquire a specialty in psychiatry in order to train in forensic or pediatric. A minimum of 11 years pass from the beginning of training to graduation in the “psychiatry” field in Bulgaria.
Published data in health reference books (Figure 1) demonstrates a clear decrease in the number of psychiatrists, from 987 in 1996 to 759 in 2016. Unfortunately, this tendency has witnessed a regrettable acceleration in the past 7 years, with a non-recoverable dropout rate of approximately 100 doctors every two years. A possible explanation of this process could be rooted in the poor workplace conditions, including the organizational and psychological climate, which tend to lead to burnout [11, 12].
Figure 1. Number of psychiatrists for the period covering 1960–2016 according to official statistics.
According to the National Statistical Institute, in 2022 there were 675 psychiatrists in Bulgaria, or 2.28% of all doctors2.
On the other hand, the Bulgarian Medical Association reports that 569 psychiatrists are active members3. Membership in the association is mandatory; therefore,it is a more legitimate source of information. The discrepancy with the Statistical Institute data is due to the fact that many individuals (real persons) are reported twice as employees. Job positions may be held in terms of two or more contracts per individual employee.
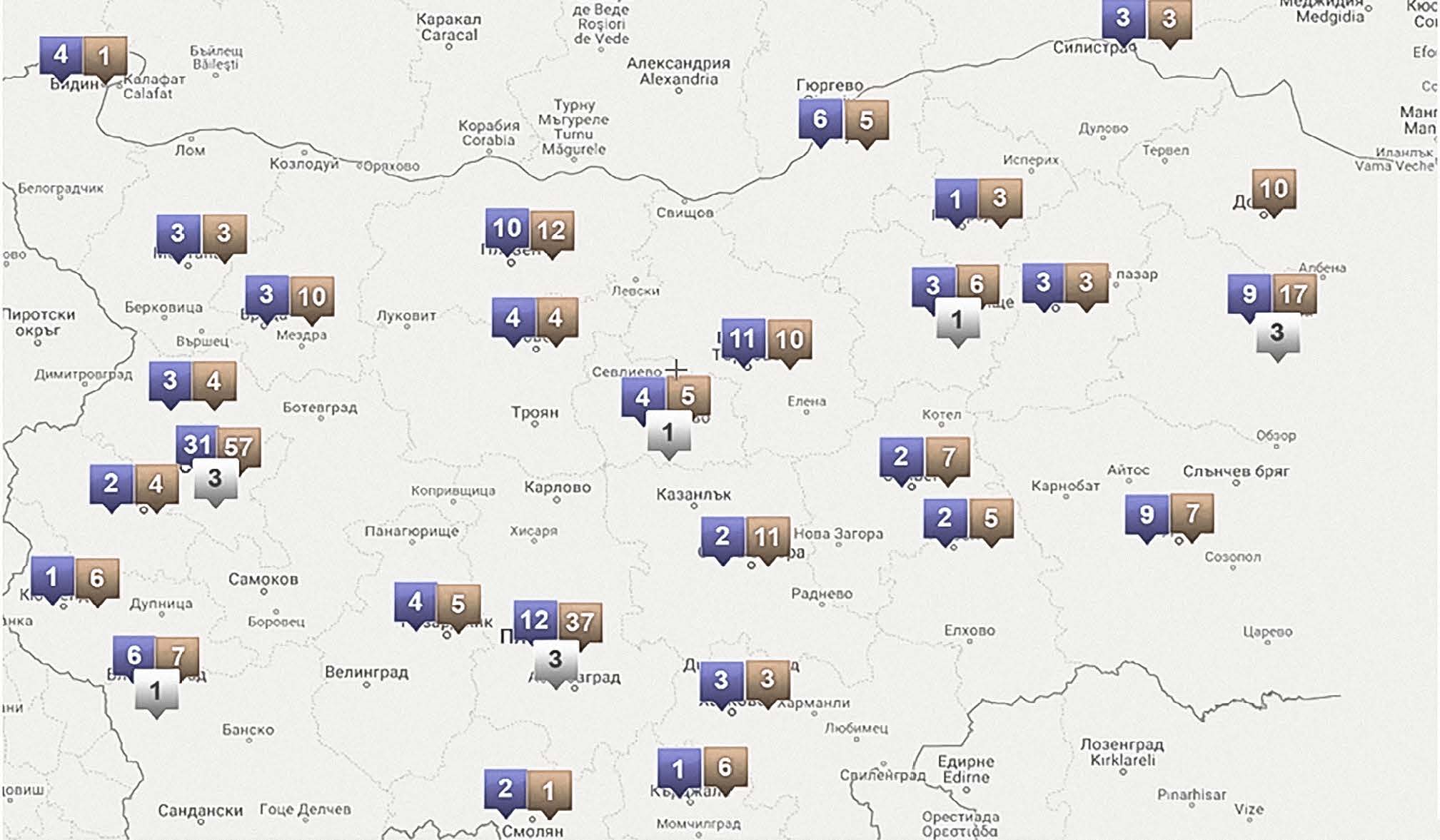
It is evident that the distribution is unequal, with certain areas suffering limited coverage (Figure 2). Besides, the average reported age of psychiatrists in the country is currently estimated at 58 years, with an expected rise to 63 years in 2028.
Figure 2. The number of psychiatrists under contract with the National Health Insurance Fund (NHIF), presumably working in the field of community care4.
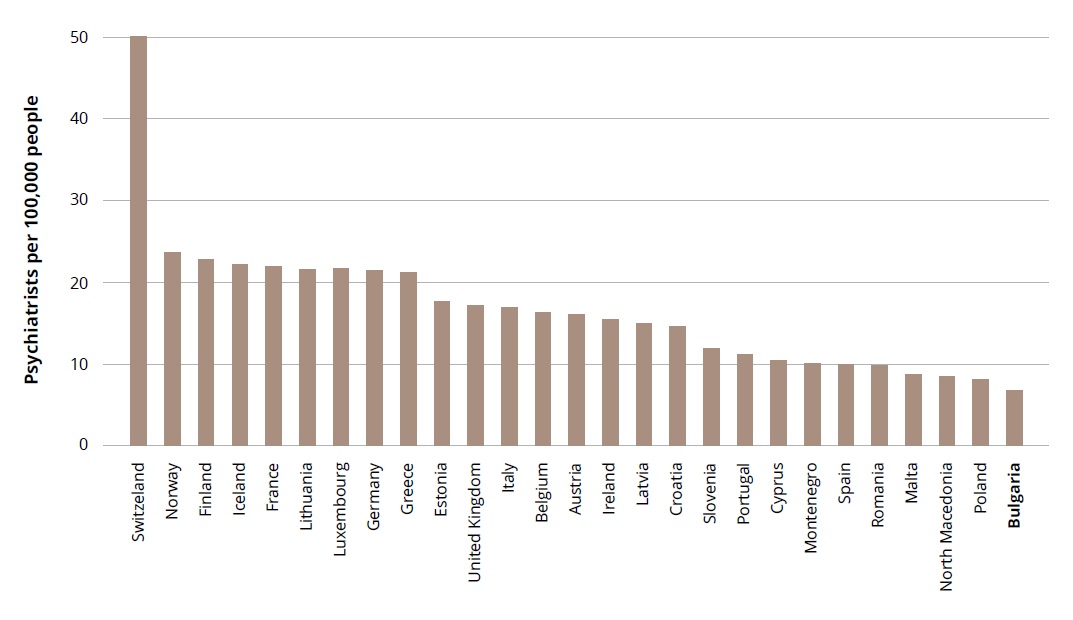
Compared with other countries in the European region, Bulgaria has an extremely diminished pool of human resources active in psychiatric practice (Figure 3).
Figure 3. Psychiatrists per 100,000 people in the EU5.
Data for other staff providing mental health services collected by the MH are from 2014. These are medical workers who practice only in inpatient psychiatric care settings. Due to the small numbers in some of the categories, we will present them in whole numbers rather than per population. Doctors assistants — 84; nurses — 1151; social workers — 56; psychologists — 134; and hospital attendants — 8306.
LEGISLATION ISSUES
Discussion about Bulgarian legislation in the field of mental health started in 2001, along with the process of accession to the EU. One of the key requirements to join the EU concerned Bulgaria’s procedure for involuntary treatment. It was debated whether to have a separate law on mental health or not. The country has never had a separate law regulating mental health, and issues such as mandatory treatment, guardianship, and legal capacity were regulated in the People’s Health Act, which was in force until 2005, when it was replaced by the new Health Act. While some experts were of the opinion that a separate law would be a form of discrimination against persons with mental disorders, others insisted that clear regulations in this field of care were necessary. In fact, the legislative system lacked the capacity to elaborate a separate law at that time and the decision was made to have a specific chapter in the new Health Act relating to mental health. The Health Act has been in force since January 1, 2005, and it governs many of the public health issues that were not covered by other recently adopted Acts, on medical facilities, and health insurance. Mental health is regulated in Chapter 5 of the Act, which has two sections, one on the protection of mental health and one on involuntary commitment and treatment [13].
ORGANIZATIONAL DISTORTION
The Health Reform in Bulgaria in 2000 launched a new phase in relationships in the system and introduced market elements in patient care, albeit largely mediated through the new health insurance institution. In psychiatry, the new conditions benefited mainly those involved in outpatient care, where the processes of services provision regulated by market forces and decentralization took place, as happened in most other medical disciplines. However, psychiatry, in its hospital unit aspect, remained outside of these processes and, thus, largely retained its institutional character. The lack of funding and managerial will to implement the objectives set out in a number of strategic documents has led to deep distortions and disproportions in the provision of mental health services. As a result, the principles of continuity of care, complexity in service, and supportive therapy have been compromised.
The paradox in the development of the psychiatric system in our country is that during the totalitarian healthcare system some form of bio-psycho-social approach was expressed through the complexes of hospitals, dispensaries, and the developed occupational therapy, although it remained firmly tethered to the practice of isolation and stigmatization of people with mental disorders. In the 1990s, this infrastructure was allowed to fall into disrepair and was largely plundered due to the lack of a well-articulated concept of reform, along with the resistance to change that came from the different stakeholders. As a result, the provision of mental health services has become chaotic, plagued by poor quality, inefficiencies, and is noncompatible to the requirements of modern psychiatric care. The few examples of good practice at some individual facilities that boast a developed rehabilitation and occupational therapy base cannot ensure a guaranteed sustainability but are rather the result of a tenuous combination of individual efforts and favorable local conditions.
New ways of treating mental disorders go far beyond pure medical intervention, which in psychiatry is largely encumbered with drug therapy and some non-medical methods — transcranial magnetic electrostimulation and electroconvulsive therapy. Such methods involve coordinated action by different groups of specialists — doctors, nurses, psychologists, and social workers — as well as the introduction of new jobs and even professions such as case manager. The lack of a comprehensive reform concept also leads to uncoordinated actions in sectors that, by definition, have to cooperate. To effect improvement, there is a need for a change in the legal framework, secure funding, and training. For now, there is still a lack of clear political will for change despite the series of strategic documents, programs, and action plans that have been adopted.
The provision of mental health services in Bulgaria relies on a combination of psychiatric hospitals, psychiatric dispensaries, and private outpatient psychiatric ambulatories.
There are 12 state psychiatric hospitals in the country, 12 Mental Health Centers (ex-psychiatric dispensaries), 5 psychiatric hospitals (in University clinics), and 17 psychiatric departments in general hospitals. The total number of beds in 2017 stood at 4,105, which is 5.8/100,000 population and represents 8.4% of all beds in the country.
Psychiatric hospitals are of an institutional type. The territorial distribution of these facilities is uneven across the country and does not take into account the migratory processes that have occurred over the last decade, as well as the transformations in socio-economic relations. Most of the hospitals are built on the basis of the isolation principle typical of the middle of the last century. The location of these institutions outside settlements does not take into account the administrative divisions of the country and does not conform to the naturally created health service territorial divisions. As a result, the patients taken in and treated in these settings are often at a significant distance from their homes, which complicates the relationship with their relatives and stands in the way of their reintroduction into society. Hospitals serve several areas simultaneously, making it difficult to manage and finance them effectively.
The 12 psychiatric dispensaries in the country are structured in a way to ensure a transition from institutional to outpatient care. Until the end of the last century, their activity was limited to the distribution of community-borne illnesses to the institution, the maintenance of an information base of patients from certain regions that are housed at the institution, and the provision of outpatient care. The psychiatric dispensaries were part of a dispensary-hospital complex housed in a basic structural unit of the institutional model. The healthcare reform has lend legal status to the healthcare institutions in the country, different forms of ownership and financing, all of which has led to the dismantling of the dispensary-hospital model. After the decentralization of outpatient care, a large part of the outpatient functions of the dispensaries was taken up by private psychiatric ambulatories, along with the documentation for patients. Many of these ambulatories signed contracts with the NHIF, and so outpatient care for insured citizens with mental disorders has continued for the most part. For a number of reasons, psychiatric dispensaries did not enter into contracts with the NHIF at the same time, and municipalities remained funded through the approved budgets of the municipalities. Instead of the former dispensaries, today Mental Health Centers have been transformed into hospitals, with a number of beds that has jumped from 25% out of the total number of beds in the country in 1989 to almost 50%.
In addition, there are small psychiatric departments in general hospitals funded by the MH through special allocations as part of a complex, mixed funding system which struggles to meet the actual needs of the population.
A large proportion of outpatient care is provided by private psychiatrists, who are funded through the national health insurance. Outpatient psychiatric care in Bulgaria is structured primarily around psychiatric individual and group practices that work independently or within another health care facility.
Across the health care provision landscape, pharmaco-therapeutic opportunities have been considerably improved in recent years thanks to the availability and use of new medicaments, especially second-generation antipsychotics and contemporary antidepressants.
Contrary to the practices in Western European countries, psychiatric treatment of severe mental diseases in Bulgaria almost entirely boils down to the application of medications, whereas other forms of treatment7 exist only in rudimentary form, where the following weaknesses have been identified as the most significant:
- there is no systematic assertive patient engagement or fieldwork;
- integration of and cooperation between parts of the medical and social services infrastructure exist in individual cases, but with no broader or systematic application;
- methods of psychosocial rehabilitation are represented partially and unevenly;
- there are no teams or sectors for intervention in early psychosis, which could be dealing systematically with secondary prevention;
- there is no clear demarcation between services according to the hierarchy of healthcare provision.
It has been universally recognized that the consequence of such tendencies is a gradual increase in the number of forensic patients.
Mental disorders are traditionally linked with rejection by society, fear, and stigma. Stigmatization of persons with mental health issues constitutes a serious problem, the consequences of which are numerous and manifest both in the experience of one’s own illness and in the diminished motivation to seek professional assistance. The stigma that comes with mental disorders is so strong that it creates a wall of silence in relation to the problem, worsens the underlying disease, and makes it even more unbearable and difficult.
Bulgaria is not an exception in this general tendency of stigmatization of individuals with mental health problems. Mental disease is still a taboo topic in Bulgarian society, not only at the individual level and the level of the families of the deceased, but also in the broader social context. Both in the local community and globally, there are attempts to debate the issue, campaigns, and other forms of de-stigmatization, but the media still devotes insufficient attention to this issue, or do it inappropriately. There are episodic manifestations to combat stigma and discrimination, on a project basis, but this is not a sustainable state policy8.
One of the major problems is the fragmentary nature and lack of continuity of both care and therapy and information about patients. After discharge from a psychiatric hospital, the patient is not routinely referred for follow-up, maintenance therapy, or any psychosocial interventions with a view to their recovery and reintegration into the community. Such activities are undertaken chaotically, depending on the particular circumstances of the patient, initiatives from their carers and family, or the local availability of services.
The complex systems that exist make it very challenging for patients to secure and continue to use treatment. For example, in order to use the services funded by the NHIF, the patient is required to visit a general practitioner, get a referral to a specialist, visit that specialist, certify the medication protocol and in the case of costly medications it must be approved by a special committee, and only after go back to the general practitioner before they can visit a pharmacy to obtain the medicines. This is likely too complicated as a setup for many patients to successfully navigate, let alone when they suffer impaired insight or cognitive functioning, or poor motivation and drive resulting from their mental disorder. Drugs for schizophrenia and bipolar affective disorder are reimbursed, but no more than at three per patient9. Anti-depressants are only partially reimbursed after one provides evidence of a depressive disorder.
One of the major challenges in psychiatric care is currently the fragmentary nature and lack of continuity of both care and therapy, as well as information about individual patients. After discharge from a psychiatric hospital, the patient is left with no regulation to follow for guidance as to follow-up, maintenance therapy, or any psychosocial interventions with a view to re-inserting them into their community. Efforts in this direction are often chaotic and depend on the condition and status of the patient, coming from a relevant outpatient service or the initiative of relatives. This state of affairs is perpetuated by the fact that a large proportion of patients that enter psychiatric hospitals are self-directed.
Social services in Bulgaria are regulated by and codified under the Social Assistance Act. There are about 6,000 beds for people with chronic disabilities in social care homes, and a small number of day care centers and shelter homes that are funded by the Ministry of Labor and Social Policy.
The existing types of social services institutions for the psychosocial rehabilitation of people with mental disabilities are Day Care Centers for Disabled Adults, Protected Homes, Social Assistance, and Home Care. The processes of deinstitutionalization in the social context, where the responsibility of the Agency for Social Assistance (ASA) begins, are still being put in place, with the European integration process of Bulgaria. As a result of these efforts, day care centers for people with mental disabilities have been opened in different areas across the country. But they work independently, unrelated to the larger medical service infrastructure, and, in smaller settlements, are confined to the immediate neighborhood. This also applies to shelter housing, access to which is not provided through the medical service apparatus, but through an order specified by the ASA. As of December 31, 2014, there are 13 shelter-like institution homes for adults with mental disorders with a capacity of 1,036 people.
FINANCIAL MANAGEMENT
The financing of health care and the system of health care reforms in Bulgaria up to this moment have been a study in transition from a Soviet model (the Semashko model10) to one that is more flexible and responsive. In the previous model, universal insurance coverage was achieved through a state-funded national health system. Doctors and other health workers we remunerated as civil servants, hospitals were allocated global budgets, and private practice and private insurance were forbidden.
Over time, Bulgaria has made progress towards a more pluralistic healthcare system based on a social health insurance model. The NHIF was established in 1999 and has become the single largest purchaser of health care services in the country. In principle, the NHIF proves to be quite comparable to many “social (or mandatory) sickness insurance funds” in the EU. In principle, the entire population is covered through compulsory and autonomous public health insurance funds. Employees (and their employers) pay into social security contributions based on their income, while the poor, the unemployed, the children, pensioners, the disabled, and other socially vulnerable or priority population groups are exempt from contributions and are covered by the state. The only existing national state fund combines health risks for the entire population and buys services both from state and private providers. The reforms also separated the purchase of services, with the idea that money follows patients, rather than funding existing healthcare facilities regardless of their activity and usage. The mechanisms for paying suppliers have been reformed; the private provision of health services and private health insurance was allowed; outpatient assistance was privatized; and hospitals became legally independent entities. The MH has retained its responsibility for public health, emergency aid, tuberculosis, HIV/AIDS, mental health, and some additional services, and its role has evolved more towards managing the system, which remains extremely financially inadequate with respect to actual needs.
Under the Health Insurance Act, insured persons are entitled to “medical assistance within the basic package of healthcare services guaranteed by the budget of the National Health Insurance Fund”. Ordinances issued by the MH — and not by the NHIF — specify the basic benefits package. The benefits package includes primary and specialized outpatient medical and dental care, medicines, diagnostics, inpatient hospital care, and some highly specialized medical services (e.g. oncology treatment, emergency aid, mental health, renal dialysis, in vitro fertilization and organ transplantation are covered by the MH). The cost-sharing requirements are different for different types of services, and insurance coverage for services is ultimately capped by the NHIF budget approved by parliament for a year.
NHIF uses a wide range of payment methods that differ for different types of providers. In general, hospitals are paid by the NHIF based on a fee in a service payment package for about 300 clinical pathways and are also subject to annual budget caps. Psychiatric care remains outside the scope of NHIF, which has no commitment to inpatient care and covers only long-term antipsychotics costs for outpatient care in psychiatry.
In summary, over the past 20 years, reform of the mental health care system has taken outpatient services from their innate function of community-based care to de facto inpatient services, with outpatient care remaining outside the scope of the overall national health insurance funding model.
PROSPECTS FOR THE FUTURE
Following an official evaluation and recommendations by the European Psychiatric Association in 201811, a National Strategy for Mental Health was adopted by an act of the Council of Ministers in 202112. The National Council was established in 2022 to guide and steer the process of its implementation. The Strategy envisages a major paradigm shift towards community-based care and seeks the appropriate funding for multidisciplinary case management in psychiatry13.
The main aims of the Strategy are briefly summarized below14:
- reducing morbidity and mortality from mental disorders by integrating psychiatric services into general medical care (deinstitutionalization);
- creating a network of integrated services for people with severe mental illnesses, in close proximity to their place of residence, centers for the treatment of disorders, and eating disorders;
- reducing alcohol and drug use and reducing manifestations of aggression and self-aggression;
- developing child and adolescent psychiatry, old-age psychiatry, and Forensic psychiatry;
- a special focus on child mental health, in line with the Convention on the Rights of the Child to ensure special protection of children’s rights, including the right to health and access to health and medical care;
- introduce a system to collect statistical information by region, type of mental illness among children, age and their analysis, including conducting targeted surveys on mental illness among children, disaggregated by age;
- develop specific measures and incentives to attract and retain specialists in child and adolescent psychiatry, forensic psychiatry, and psychiatry of advanced age;
- restore the balance between individual psychiatric professionals, social worker’s psychologists, nurses, and orderlies with the development of appropriate incentives to attract professionals;
- respect human rights and combat stigma and discrimination.
Currently the National Strategy is under implementation and monitoring.
CONCLUSION
In conclusion, it can be said that in recent years the Bulgarian mental health care system has not changed much and still has a long way to go. Despite the socio-economic difficulties in the country, the system needs to evolve to improve the level of care provided to patients. Bulgaria should take active part in as many international projects as possible aimed at introducing better treatment practices in the community for patients with mental disorders. More importantly, Bulgaria must invest in mental health education, in preventive psychiatry, and in developing a culture of clinical management and organization. It is necessary to encourage Bulgarian society to play an active role through education and information in the fight against the stigma of mental disease.
1 It is taken by implication as Soviet state socialism, as other forms of socialist health care, such as the Scandinavian model, are outside the scope of this paper.
2 The National Statistical Institute [Internet]. Doctors by specialties in medical and health care institutions on 31.12.2022 by statistical regions and districts. [cited 2023 June 8]. Available from: https://www.nsi.bg. Bulgarian.
3 The Bulgarian Medical Association. National Register of doctors affiliated to the union by gender, age, specialty and place of practice [cited 2023 June 8]. Available from: https://blsbg.eu/en.
4 The National Health Insurance Fund. Available from: https://nhif.bg/.
5 Eurostat data for 2015.
6 The Ministry of Health Republic of Bulgaria. Internal report from the 28 regional health inspectorates. Not published.
7 Such as mobile psychiatric care, telemedicine, transcranial magnetic stimulation, some forms of occupational and art therapy. Even traditional forms such as electroconvulsive therapy are complicated.
8 National Center for Public Health and analysis. Project „Improved mental health services”. Available from: https://bgmental.ncpha.government.bg/en/node/35.
9 The NHIF has drug reimbursement rules that do not allow more than three drugs to be paid for an illness. It is necessary that these indications for the prescription of medicines be explicitly stated in the summary of product characteristics.
10 Soviet model of Nikolay A. Semashko, a centralized budget-funded and regulated system, which claimed to guarantee “free access to health services for the entire population”.
11 European Psychiatric Association Report on Bulgarian Mental Health care and Reform Process 2018. Available from: https://www.europsy.net/app/uploads/2019/01/EPA-Bulgaria-Report-2018-Final.pdf.
12 https://www.mh.government.bg/media/filer_public/2021/11/02/21rh388.pdf.
13 Case management is the coordination of community-based services by a professional or team to provide quality mental health care customized accordingly to individual patients’ setbacks or persistent challenges and lead them to recovery. Case management seeks to reduce hospitalizations and support individual recovery through an approach that considers each person’s overall biopsychosocial needs without incurring crippling economic costs. As a result, care coordination includes traditional mental health services but may also encompass primary healthcare, housing, transportation, employment, social relationships, and community participation. It is the link between the client and care delivery system.
14 National strategy for mental health of the citizens of the Republic of Bulgaria 2021 – 2030. Available from: https://www.mh.government.bg/media/filer_public/2021/11/02/21rh388pr1.pdf.