INTRODUCTION
Over the past 20 years, many advanced technologies have emerged that have significantly expanded our knowledge of the brain and the neurobiology of mental disorders. At the same time, a lack of new biology-centered knowledge precludes a real breakthrough in applied neuroscience [1].
Moreover, against the background of rapid progress of medical technology, psychiatry has demonstrated, over the past two decades, an apparent conceptual diagnostic and therapeutic crisis due to the loss of the vector for further development of both theoretical research and clinical practices, which are a natural extension of the theory [2–8]. The fact is that the considerable advances in neurobiological technologies have narrowed the view of many psychiatrists, who eventually focused on conducting exclusively biomedical research aimed primarily at studying the biological basis of psychiatric diseases. As a result, the concept of mental illness as a disorder affecting the entire psychophysical system, which was established in psychiatric science during the 19th and 20th centuries, is being reduced. This complex picture is being transformed to a simplified view of “brain diseases” [9, 10]. Prioritizing genetic, as well as neuroimaging and cognitive research, proponents of this approach essentially postulate a neurobiological paradigm of psychiatric disorders (in which the understanding of their nature borders on Democritus’ atomistic-materialistic conception), ignoring the dualistic organization of the human psyche (first mentioned by Aristotle), which in modern times is viewed according to the framework of psychophysical parallelism (using the terminology of Gottfried Wilhelm Leibniz).
The most obvious manifestation of the crisis in psychiatry at the beginning of the 21st century, as a result of its pronounced “biologizing bias”, was the fact that the theoretical and practical potential of the categorical principle in the diagnosis of psychiatric disorders had been largely exhausted by the end of the 20th century [11, 12]. As a result, the strict demarcation of exogenous-endogenous relationships was abandoned in favor of conceptions of the spectra of mental disorders. At the same time, even with this “updated” approach, psychiatric terminology, in fact, remained disconnected from the actual person suffering from the particular mental illness.
As a result, psychiatry as a science in which the natural scientific and humanitarian components are in an unbreakable unity (which corresponds to the unity of man as an indissoluble psychophysical phenomenon) is being transformed into a purely technocratic science focusing on certain clinical manifestations, rather than on the person. In turn, the subject-subject relationship that underlies the medical care delivered by the physician to the patient turns out to be an exclusively subject-object one. In other words, psychiatry as a science becomes a technology, which leads to its dehumanization.
Emphasis here must be placed on the following. Once the development of psychiatry, which led to the emergence of concepts of “spectra” of psychiatric disorders and their dimensional (quantitative) assessment allowing in many cases the determination of the severity grade of a particular psychopathological domain. On the other hand, in isolation from the further development of the categorical approach, this quantitative assessment is far from helping to a achieve tangible breakthrough in the current clinical and diagnostic crisis and turns out to be one of the its aspect.
The fact is that dimensional diagnostic constructs are ineffective in the absence of a fully updated theoretical basis. They do not allow for a comprehensive theoretical approach, because they are based on an arbitrary conventional and simplified eclectic approach that describes psychiatric disorders without taking into account individual features and the psychological history of the individual.
With this approach used in practice, especially in the treatment of mental disorders that not associated with stress, it is limited to the use of psychotropic drugs, which destroys both the comprehensiveness of therapeutic efforts and the system for evaluating its effectiveness. Moreover, last mentioned is reduced only to documenting a decrease in the severity of certain full-blown psychiatric syndroms. In turn, this means that the treatment efficacy assessment suffers from an extremely wide and uncontested use of evidence-based criteria obtained solely on the basis of randomized scientific studies of psychopharmacological medicines.
Today, study designs are focused on symptomatic improvement methods implemented through randomized controlled trials (RCTs). At the same time, the significance of the efficacy indicators proposed based on RCTs is not ranked or at least clearly defined [13].
A simple review of the literature can easily detect a significant quantitative prevalence of randomized clinical trials investigating the efficacy of pharmacological interventions over studies of non-pharmacological interventions [14].
The question is, should we rely solely on statistical analysis of numerical data, as is the case with randomized controlled clinical trials [15]? Is it possible to increase the proportion of psychosocial systematic empirical studies relevant to clinical practice, in which psychological interventions are used along with drug therapy [16, 17]?
DISCUSSION
The main criticisms of the results obtained in psychiatry through the use of RCTs and other evidence-based methods concern its three main drawbacks:
- Excessive dependence on experimental biological (genetic, pharmacological, etc.) empiricism [18], which reflects a rather superficial level of relationships in contrast to theoretical approaches that reveal essential connections of reality;
- An erroneous t understanding of the very term “evidence” [19];
- Doubtfulness of the idea that the basic provisions of evidence-based medicine are the only ones that can be correct [20].
It should be noted that Russian psychiatrists, who have taken the path of evidence-based medicine, are often extremely narrow and rigid in their interpretation of the approach based solely on high-quality RCTs, while at the same time maintaining that this is the only possible approach. According to this approach, identified general patterns observed in a small cohort of specially selected patients are declared axiomatic for a whole spectrum of psychiatric disorders, without taking into account individual characteristics of patients. As a result, the main methods in the evidence-based medicine system are statistical methods [21], despite the fact that establishing a statistically average probability is a scientific-statistical, but not a scientific-systematic approach [22], and that improving statistical procedures is unlikely, first, to advance the understanding of psychiatric disorders and, second (no less important), to improve the outcome for a particular patient [23].
In addition, ardent proponents of the evidence-based approach essentially deny the value of author expertise as an important source of relevant knowledge. This means that both expert opinion (based on clinical thinking and the personal professional experience of the physician) and the specifics of the individual adaptive and compensatory potential of a particular patient are left out. In particular, descriptive reviews reflecting the personal positions of the authors of a publication on a particular problem are assessed by evidence-based medicine practitioners as “low-grade”, contrasting them with systematic reviews as the result of serious scientific research [24]. It is easy to see that this is nothing more than a very vulgar and far from scientific attempt to “rank” completely different types of scientific research, each of which has its own set of “limits” inherent in the research algorithm itself.
As a result, many doctors (not only psychiatrists) are simply made to believe that truly scientific and trustworthy evidence can only be based on experimental material and, moreover, it must be thickly, layer-by-layer embalmed with mathematical formulae that probably guarantee such evidence eternal value and immortality. This kind of idea has also become popular with Russian specialists in the field of psychiatric and behavioral disorders, although the relevant section of the current classification ICD-10 is not a product of evidence-based medicine, but a compromise convention) [25].
It must be underlined that the principle of Cochrane evidence1 is interpreted more broadly in the West than by the majority of its Russian adherents. Many Western proponents of RCT (EBM) consider evidence-based medicine to be centered on the patient’s personality as a whole, rather than on fragmentary symptom-related indicators tested in biological experiments. From this point of view, evidence-based medicine appears to be a process of providing medical care that involves the accumulation, interpretation, and integration of reliable, important, and reasonably applicable evidence that serves to improve the quality of clinical decisions regarding the treatment of a particular patient [26].
A number of Western, as well as “moderate” Russian, supporters of Cochrane evidence harbor the idea that both RCTs and the analytical processing of their data always require the consideration of a number of factors known to limit the relevance of evidence-based medicine methods and necessitate additional control and retesting of results obtained through RCTs (EBM). These factors are:
- The efficacy-effectiveness gap, which remains the Achilles heel of evidence-based academic approaches [27]. There are differences between the benefits of a drug intervention in a simulated setting (RCTs) and in real-world practice [22]. This situation calls into question the absolute validity of the results of RCTs that have demonstrated the efficacy of certain drugs [28].
- Lack of a universal approach to demonstrating a direct relationship between the individual approach and median RCT data [22]. This results in limited utility of reliable RCT results for individual patients [29], as these studies do not take into account the fact that “statistical results obtained in randomized controlled trials (RCTs), systematic reviews and meta-analyses are of little use for decision-making regarding individual clinical cases, as they provide only a probabilistic answer to the questions and do not take into account individual patient characteristics” [30]. Even setting aside the question of potential diagnostic errors in RCTs, it seems quite clear that RCTs, which use average group values, do not provide answers to questions about the treatment of individual patients [29]. The existing tools for therapeutic choice involving RCT data (assessment of sample size, benefit-risk profile, characteristics of adverse outcomes in the test and control groups, etc.) do not allow for prediction with a high probability of any actual impact of the treatment on an individual patient, who is not a hypothetical “average person”. In other words, general patterns identified in randomized trials (the effectiveness of a particular drug in certain psychiatric conditions) cannot be taken as axiomatic for an individual case (individual patient). It is natural then that evidence-based medicine is suggested as a variant of species survival strategy, whereas clinical practice is suggested as an individual survival strategy [31]. It is also important to emphasize that the failure to take into account the conditionality of conventional diagnostic distinctions in the assessment of RCT results leads to unjustified absolutization and excessive generalization of conclusions regarding the efficacy of particular therapeutic interventions in a wide range of psychiatric disorders. Finally, RCTs study “ideal patients” whose proportion in the population does not exceed 5–10%. At the same time, study results obtained in a small, clinically refined group of conditions are subsequently extrapolated to all patients and serve to justify standardized treatment for a large group of conditions, and without taking into account the individual features of the patient. Yet averaged efficacy and tolerability indicators obtained in the course of evidence-based studies may prove useful, useless or even harmful in the treatment of a particular patient.
- Methodological impossibility of conflict-free (impartial) use of the evidence-based doctrine in psychiatric practice [8, 32, 33]. This factor has to be placed here, because it is impossible to completely exclude its role due to the influence of pharmaceutical companies on the results of clinical trials, despite all the measures taken to counter this impact [34]. It is common practice for practitioners — who are under the direct influence of pharmaceutical companies — to ignore evidence supporting the efficacy of older treatments while actively encouraging the use of new, more expensive therapies [14]. According to Every-Palmer and Howick [28], it is often the case that opinion leaders advocating the value of trial evidence are also paid specialists of the marketing departments of pharmaceutical companies. The obvious conflict of interest means that their conclusions cannot be perceived as scientifically objective. Furthermore, even clinical recommendations based on the individual authority of investigators, who are directly or indirectly associated with pharmaceutical companies, cannot be free from suspicion of bias. Pharmaceutical companies are also known to use many indirect ways to influence choice of treatment. There is still no satisfactory solution to these issues of the qualitative analysis of study results.
- In medical practice, including “evidence-based” studies, complete elimination of the role of the physician’s personality (“charisma”) accumulating their individual education and medical experience, empathy, and intuitive judgments is unlikely (and in reality impossible).
As noted by Zobin and Ustinova [22], these factors complicate the unification of therapeutic choices if it is based solely on the data obtained during RCTs. This does not mean, however, that the relationship between evidence-based medicine and psychiatric practice cannot be discussed in terms of the dialectical interaction of the general and particular.
It appears that the total and dominant use of evidence-based medicine principles is insufficient in the context of a biopsychosocial diagnostic approach, which includes a multi-dimensional (multi-vector) view of treatment efficacy criteria. It involves a differentiated examination of the patient’s clinical, psychological and social status. The “refined” postulates of so-called evidence-based medicine cannot always be used as a means to determine the most effective option of therapeutic intervention [2]. Evidence-based medicine should also be used very carefully in the evaluation of psychosocial and “client-centered” interventions, where existential factors that can by no means be described by RCTs must always be considered as very important.
In addition, attempts to determine the strength of evidence for various psychotherapy methods also appear unsuccessful. Where evidence-based medicine methods — despite both scientific and simple common sense — are still considered as the only method appropriate to the determination of the efficacy of non-drug (in particular, psychotherapeutic and sociotherapeutic) interventions and organizational rehabilitation measures, these methods often turn out to be not just useless, but even harmful. It should be repeated here that the founders of the evidence-based concept never declared that their method was unique or indispensable in all diagnostic and therapeutic scenarios without exception.
That said, evidence-based medicine does have its own strengths, and initially it was not meant to do away with the traditional paradigm (a “cuckoo chick” pushing out competitors out of the nest), but was instead intended to be a means of universal assistance in expanding clinical experience and making informed therapeutic decisions [35], that is, decisions stemming, firstly, from the physician’s individual experience and, secondly, from data obtained through the analysis of large bodies of diverse clinical evidence. Evidence-based medicine methods appear to be effective primarily in choosing the appropriate treatment for biologically determined components of mental illness (including the choice of medication). It is these aspects of the nature and purpose of evidence-based medicine that meet “clinicians’ desire to obtain more detailed information for the choice of treatment options in real-world clinical practice” [30].
In addition, it should be emphasized that the alternative to evidence-based medicine, i.e., the subjective expert (individual physician-centered) approach is also vulnerable and should by no means be viewed as the only effective tool. The weaknesses of this approach are as follows:
- There is still no satisfactory solution to the problem of inclusion of subjective characteristics (based on the clinician’s perception of external data and personal wishes of patients) in a formalized clinical decision-making protocol.
- A clinician’s assessment of the efficacy of various treatments is largely determined by their analytical abilities, depth of understanding of the methodologies of different study designs, and knowledge of basic statistical procedures. That is, it depends on many subjective factors that collectively contribute to the physician’s art, which, ideally, is a properly calibrated body of evidence, expert conclusions, and clinical experience [36].
- The patient’s needs are also difficult to systematize, as they are determined by their personal preferences, individual psychosocial characteristics, and specifics of the therapeutic alliance [23]. Additionally, the declared need to take into account the patient’s preferences and values when choosing a treatment in psychiatry is limited by the potential inability of the patient to adequately assess their condition due to the nature of the disease itself. It should be added that the mentioned right of the patient is limited not only by their competence, but also by objective factors related to the complexity of interpretation of the evidence.
And yet, despite the mentioned limitations of the subjective expert (individual physician-centered) method, it is the physician who remains the integrator and guide in the search for optimal clinical solutions and therapeutic choice. As a result, it is still firmly believed that the search for the most effective therapeutic intervention in psychiatry should be guided not by a formal protocol, as recommended by the strict rules of evidence-based medicine, but by an expert consensus that should be in agreement with the protocol. The absence of such agreement only increases the risk of the basic provisions of the evidence-based approach being compromised [23]. In these cases, therapy is sometimes reduced to strict compliance with the prescribed pharmacologically focused “standards”, that is, in most cases, reduced to a routine prescription of the required drugs “legalized by classifications” as the only adequate means of treating specific clinical forms of the disease. Thus, the treatment of the condition becomes disconnected from the integrated nature of the mental disorder, that is, only the patient’s disease is treated rather than the patient themselves.
All of the above — at a new level of understanding — brings us back to the statement at the beginning of the article of the crisis state psychiatry is now in due to the conflict of the purely biomedical model supported by pharmaceutical companies and still prevailing in practical medicine and the biopsychosocial model, which, in reality, is maintained only by some scientists and practitioners.
As follows from the facts and generalizations discussed above, this conflict is more subjective than objective and should be resolved as soon as possible and completely. The point is that biologizing approaches are fundamentally insufficient to achieve the final goal of providing the most effective comprehensive therapy for mentally ill patients and achieving their functional recovery, if the humanistic approaches are completely ignored. Similarly, humanitarian approaches are insufficient if they are completely “disconnected” from the neurobiological basis and operational criteria. At the same time, the biologizing and humanistic approaches (based on the biopsychosocial paradigm) appear to be in unequal conditions. The former, receiving financial and lobbying support from pharmaceutical companies, are actively being implemented. The latter, due to the lack of lobbying, are being increasingly isolated from current psychiatric practice, which appears to be almost entirely focused on psychopathological diagnosis and the introduction of purely psychopharmacological treatments.
As an interim summary, it should be emphasized that the two strategies being discussed cannot be “reconciled” or combined. Furthermore, they do not follow from each other and do not form a hierarchy. They are always parallel and complementary. It is only necessary to be aware of their purpose and make sure that one of these approaches does not destroy the other in order to facilitate vulgar ideological simplifications covered by references (often incorrect) to “authorities” or promote the commercial interests of pharmaceutical companies.
A particular patient combines features of both the general (species) and the single (individual). Since there are no absolutely identical or completely different patients, opposing evidence-based approaches on the one hand and clinical practice on the other makes no sense [23]. Nor do the attempts to declare “monopolism” of any of them.
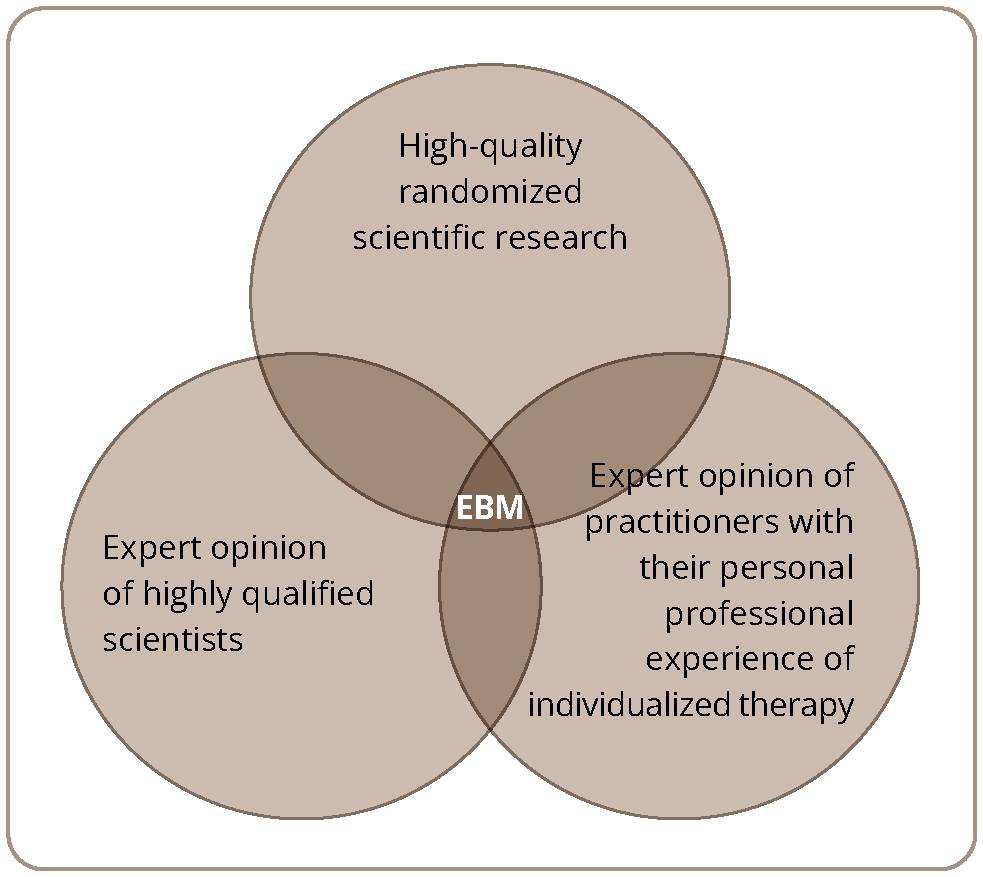
These considerations elucidate increasingly clearly that evidence in medicine must — in order to be purely beneficial — include 3 mandatory intersecting components (Figure 1).
Figure 1. Scheme representing the evidence-based medicine (EBM) “triad”
As can be seen, to be justified, evidence-based medicine must take into account the following data:
- high-quality randomized scientific research,
- expert opinion of highly qualified scientists (it should be noted here that the methodological error of the strictly understood Cochrane evidence principle is in the fact that the competencies and expertise of particular specialists are subtly excluded from the “evidence-based medicine” system itself),
- expert opinion of practitioners whose experience allows for the discovery of the individual adaptive and compensatory potential of patients and take it into account during treatment.
In this regard, a promising type of study would be one that involves a mutually beneficial “cooperation” of these three components of evidence, which can form the basis for the development of a biopsychosocial understanding of the nature of psychiatric disorders, their holistic diagnostic assessment, and the development of comprehensive therapeutic options, as such studies would not be limited to the consideration of the biological mechanisms of the disease.
CONCLUSION
Modern medicine, as we have already pointed out earlier [37], seeks to approach the exact sciences in many ways, but will still never become one of them. The fact is that the expert judgment of a physician (be it a scientist or a practitioner) based on their individual experience and their personality, as well as their knowledge of the features of the patient, has always been and will be important for effective treatment, which, in turn, is the main goal of medicine both as a science and as a practical activity. It should be further emphasized here that in the field of psychiatry, the evidence-based medicine principles positioned to turn out to be the farthest (compared with other medical specialties) from the complex nature of the disorders being studied and, therefore, from the right to be considered a monopoly approach to treatment effectiveness assessment.
Evidence-based medicine in the strict sense is not equivalent to medical evidence. Currently, there is a clear polarity of views about the use of RCT results in healthcare practice. The bias towards the evidence-based medicine principles takes on another negative aspect in our current situation, when pretext of the absolute value of “evidence” is used to “optimize” treatment and healthcare. This leads not only to a decrease in the availability of a wide range of specialized medical care, including psychiatric care, but also to a deterioration in its quality (due to the practical reduction of therapy to the use of psychopharmacological drugs only). As a matter of fact, psychiatry is losing clinical ground.
We need a constructive convergence of the two points of view. On the one hand, it must be admitted that a clinician who does not use RCT data is like a traveler without a compass and a map. On the other, however, it is also clear that a physician who blindly follows the “evidence-based” standards and does not have their own clinical experience, not taking into account the individual features of the patient, is like a traveler, although with a compass, but in an area of magnetic anomaly. Because of this, both physicians relying only on their personal experience and common sense (expert opinion) and physicians treating exclusively “according to what is written” in meta-analytical reviews (high-quality research studies) are equally alarming: even if you regularly read the most up-to-date systematic reviews (which are an ultimo ratio from the point of view of evidence proponents), it is the physician who, as Trisha Greenhalgh correctly observes [38], “must decide how this quantitative result, significant or non-significant, will affect the treatment of this patient”. And although the methods of evidence-based medicine, when used to assess the efficacy of psychotherapy, require an extremely complicated RCT protocol (and, it seems, completely rule out the use of the double-blind design due to ethical and pragmatic considerations), they do not cancel out the “universal evidence-based” concept itself, which is aimed at the “absolute” reproducibility of results.
We would like to conclude this discussion of the prospects of “removing” the basically artificial opposition and conflict of the evidence-based paradigm in the assessment of the effectiveness of diagnostic and treatment options, on the one hand, and the expert-oriented paradigm, on the other, as well as of the urgent need for the establishment of their mutually beneficial “cooperation”, with a philosophical generalization of Yu.A. Aleksandrovskiy [39], which reveals the mutually complementary “solidarism” of all living beings, including the scientific description and understanding of these living beings: “The evolutionary, multi-century association of living cells and the formation of the simplest, and then complex, animal and human organisms are vital to the interaction process, despite temporary situational confrontations. With this in mind, we can think of the need to create a unified general theory of integration and development for both biology and sociology”. What has been said seems extremely topical and focuses our attention on the need to develop, as soon as possible, a full-fledged theory of evolutionary psychiatry and integrative methodology in order to synthesize biological psychiatry (as a natural science) and psychosocial psychiatry (as a largely humanitarian science), as comprehensive therapeutic efforts cannot be successful without this. In this case, the evidence-based approach, with a moderately critical attitude to it, can become valid for all types of research studies.
In connection with the above, we have to agree with the D.A. Zateyshchikov [40] that, since variability is the law of life and there are no two identical organisms or two people with identical diseases, we should proceed from evidence-based medicine to individualized medicine, since evidence-based medicine “treats not the patient, but the population, i.e., it decreases the incidence rate in the population as a whole”. Especially dramatic in this context is the issue of technological depersonalization and objectivist neglect of the mental patient’s psychological identity in the current system of “evidence-based digital” psychiatry [41]. This negative trend makes the important, although non-specific, aspects of treatment (such as the patient-perceived quality of the treatment alliance) secondary, while the culture and meanings of this alliance are often key to how the characteristics of the patient’s mental state change over time [42]. Therefore, the focus on the person-centered (individualized) approach to the patient is becoming particularly important.
Thus, the future lies in the targeted development and evidence-based consideration of the effects of therapeutic interventions on the mechanisms of pathogenesis of psychiatric disorders, including the study of cause-effect relationships between their constituent biopsychosocial domains. The choice of therapeutic intervention, as well as the assessment of its quality, should be based on a person-centered, individualized approach to the patient that should be in agreement with the biopsychosocial views on the development of psychiatric disorders. This approach implies that the patient is treated not only as an object (even if only a single object), but also as a subject with a complex inner world. It goes without saying that the role of the “humanistic component”, in addition to natural science and biology, is extremely significant for certain fields, such as psychology and psychiatry — the latter having a rehabilitative function that clearly requires the use of psychological and social therapy in addition to psychopharmacology.
1Cochrane Collaboration is a registered not-for-profit organization involved in the development of World Health Organization guidelines. The name of the organization comes from the last name of its founder, the Scottish medical scientist Archibald Cochrane (Archibald Leman Cochrane, 1909–1988), who advocated evidence-based medicine and clinical trials and wrote the book Effectiveness and Efficiency: Random Reflections on Health Services (Cochrane Archie, 1972).