INTRODUCTION
Computational psychiatry (CP), a rapidly evolving field, is often defined in various ways across the literature. For the purposes of this review, we align with the definition proposed by Montague et al., viewing CP as an interdisciplinary field that leverages mathematical models and computational algorithms to understand, predict, and enhance mental health [1]. This broad scope encompasses the modeling of neurobiological processes, the application of machine learning in the predicting of psychiatric states, and the development of computational tools to aid clinical practice. Under this umbrella, ‘aspects of computational psychiatry’ in our review refer to any research or applications that employ these approaches in the study of mental health.
In this narrative review, we aim to offer an insight into the current landscape of CP, discussing its significant challenges, as well as the potential opportunities for the field’s growth. By highlighting the essential role of interdisciplinary collaboration and ethical safeguards, we hope to contribute to the ongoing discourse surrounding the responsible development and application of computational approaches in psychiatry.
It is important to stress that overcoming these challenges will be a demanding, yet crucial endeavor. The potential of computational psychiatry to transform mental health care inspires us to confront these obstacles and facilitate the field’s progression with care, diligence, and due consideration for ethical implications.
METHODS
The authors have carried out a narrative review of the scientific literature published on the topic of CP. Both theoretical articles and published research results up to and including May 2023 were considered in the review. The literature search was performed in the PubMed and eLibrary databases, as well as PsycINFO and Google Scholar to ensure a comprehensive review. The following keywords were used to search for the scientific literature: “computational psychiatry”, “digital psychiatry”, “digital mental health”, “computers in psychiatry”, “artificial intelligence in psychiatry”, “AI in psychiatry”, “machine learning in psychiatry”.
The evaluation of articles was performed by two independent reviewers, who assessed the publications based on predefined inclusion and exclusion criteria. Any disagreements between the reviewers were resolved through discussion until a consensus was reached. Articles were deemed to fulfil the inclusion criteria if they focused on aspects of CP and the full text of the article was available to the authors. In addition to articles, books that proved significant contributions to the field were also considered. Additional search was conducted in the reference lists of the articles included in the analysis.
A descriptive analysis was used to summarize the published information on the theoretical and practical aspects of CP. In total, our review includes 54 publications, providing a broad overview of the current state of CP.
RESULTS
In our exploration of the field of CP, we have identified several key themes that recur in the literature. These themes include the definition and scope of CP, the challenges and ethical considerations it presents, the role of interdisciplinary collaboration, the recognition and growth of the field, its application to specific psychiatric disorders, and potential future directions. These themes provided the framework for our discussion of the literature and helped to highlight the key points made by various authors. In the following sections, we present a summary of our findings for each theme, aiming to provide a balanced overview of the current state of CP.
Definition and scope of computational psychiatry
Computational psychiatry is an emerging interdisciplinary field that aims to integrate computational modeling, empirical data, and theoretical insights from various fields, such as psychology, neuroscience, computer science, and mathematics, in order to better understand psychiatric disorders and their underlying mechanisms [1, 2]. The central goal of this field is to develop quantitative models that can link neurobiological processes, cognitive functions, and clinical symptoms to improve diagnostic accuracy, identify novel therapeutic targets, and predict individual treatment responses [3, 4].
To achieve these aims, CP researchers employ a variety of approaches, including reinforcement learning [5], Bayesian inference [6], dynamical systems theory, information theory [7, 8], and large-scale data analysis and network modeling [9, 10]. These approaches help in the investigation of the complex and dynamic nature of psychiatric disorders, dysfunctions in learning and decision-making processes, and the interactions between different brain regions and genetic and environmental factors.
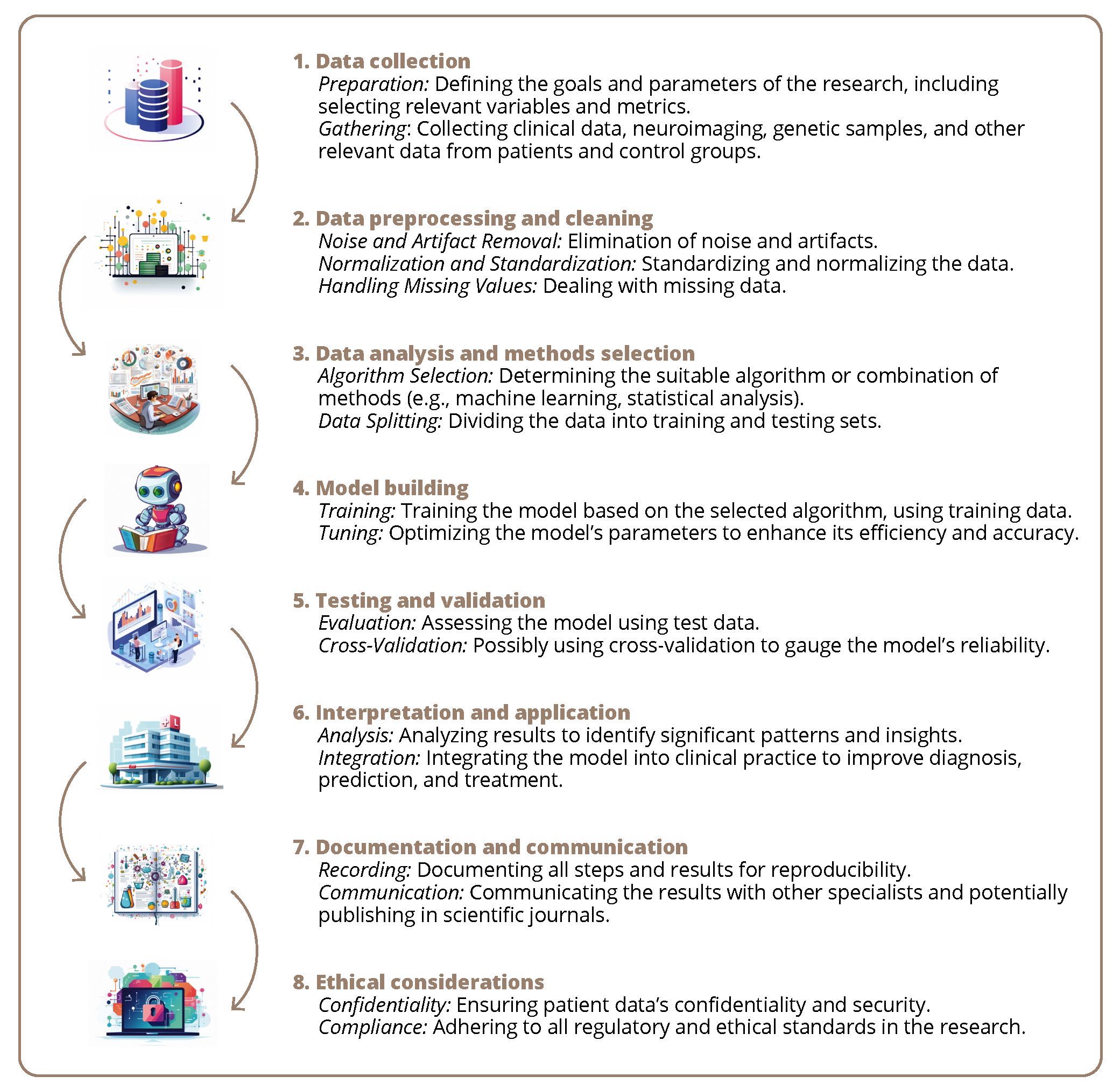
A key challenge in CP is to develop computational models that effectively reproduce the complexity of psychiatric disorders and account for individual differences in symptomatology and treatment response [11]. This process often follows a generalized schema that includes stages such as data collection, preprocessing, modeling, testing, interpretation, and ethical considerations. A detailed illustration of this process can be found in Figure 1.
Рисунок 1. Обобщенная схема разработки вычислительной модели в психиатрии: обзор.
The integration of various computational approaches can enable researchers to develop more sophisticated models and test specific hypotheses regarding the mechanisms underlying psychiatric disorders [12]. Moreover, CP benefits from advances in machine learning and artificial intelligence (AI), providing novel ways to analyze and interpret complex psychiatric data and offering potential avenues for personalized treatment [13]. The application of computational approaches to neuroimaging data further advances our understanding of the neural basis of various psychiatric disorders [14].
The success of CP ultimately depends on close collaboration between computational scientists, neuroscientists, and clinicians, as well as the development of rigorous model validation and evaluation techniques [15]. By providing a quantitative framework for understanding mental disorders, CP helps to bridge the gap between clinical observations and neurobiological mechanisms, ultimately contributing to the development of more targeted and effective interventions [2, 16].
Interdisciplinary collaboration
Interdisciplinary collaboration is a cornerstone of CP, as it blends insights from various fields such as psychology, neuroscience, computer science, and mathematics to better understand psychiatric disorders and their underlying mechanisms [1, 2]. This cooperation is not without its challenges. For instance, the integration of different methodologies and theoretical frameworks can be complex and requires a deep understanding of multiple disciplines [16]. However, the potential benefits of such teamwork are significant: it allows for the development of more comprehensive models of psychiatric disorders, which can lead to improved diagnostic tools and treatment strategies [17–19].
Moreover, interdisciplinary efforts extend beyond the scientific community. They also involve the education and training of mental health professionals. This includes not only equipping them with the necessary computational skills, but also fostering an understanding of the potential benefits and limitations of computational approaches [20–22].
The essence of interdisciplinary work in CP is also reflected in the research practices within the field, especially in the context of omics technologies. These include genomics, as well as emerging fields such as lipidomics, proteomics, and transcriptomics. Polygenic disease genetics, for example, is one of the omics models, with approaches like polygenic risk scores at the forefront. The application of these multimodal approaches, in conjunction with big data analysis, is mainstream in computational research, significantly contributing to the modeling of mental illnesses [23–26]. This integrative approach is essential for the advancement of CP and its application in clinical practice [27–29].
Challenges and ethical considerations
Despite the promising potential of CP, the field faces several intricate challenges. One primary hurdle is the development and interpretation of computational models that accurately reproduce psychiatric disorders, accounting for individual differences in symptomatology and treatment response [11]. Integration of various computational approaches can lead to more sophisticated models but brings forth difficulties in double-checking, verification in independent studies, comparison in multi-center studies, and across populations, possibly resulting in inaccurate or tainted conclusions [30].
Furthermore, mathematical models, particularly those using big data and machine learning, calculate probability values, such as risk degrees [31]. Misunderstanding these probabilities can lead to societal judgments, especially when personal data leakage occurs, equating risk with diagnosis and potentially leading to stigmatization [32].
The complexity of these models also necessitates the development of stringent guidelines and standards, which becomes crucial in the context of CP [33]. The preconceptions and apprehensions surrounding computational technologies must be overcome. Emphasizing model transparency and biological plausibility can facilitate more widespread acceptance and use [11, 12]. Addressing these challenges, including ethical considerations, will be vital for the continued growth and success of CP in mental health care [28].
Recognition and growth of computational psychiatry
Computational psychiatry, lying at the intersection of neuroscience, psychiatry, and computer science, has been recognized as a significant area of scientific knowledge since the mid-1980s [1, 17]. Despite the complexities and challenges associated with the integration of computational technologies into practical healthcare, the field has seen substantial growth over the past few decades [34]. The evolution of CP heavily relies on the synergy between computational scientists, neuroscientists, and clinicians. This interdisciplinary collaboration is essential to develop a comprehensive understanding of mental disorders, improve diagnostic accuracy, identify novel therapeutic targets, and predict individual treatment responses [1, 2, 16].
The potential of computational technologies in psychiatry has been recognized since the pioneering work of Hedlund et al. (1985) [34], who were among the first to highlight both the potential and challenges associated with this integration. Despite the more than decade that has passed since the first mention of computational psychiatry in publications [1], substantial changes in the field appear to be minimal. However, the advancement of computational psychiatry heavily relies on the synergy between computational scientists, neuroscientists, and clinicians.
The recent integration of machine learning and AI into computational psychiatry has only served to intensify this sense of potential and novelty, offering unparalleled means to dissect complex psychiatric data [13]. However, there is still a palpable misunderstanding within both the literature and professional communities about these technologies. In particular, the apprehensions surrounding the utilization of computers by specialists persist, including the use of modern technologies in psychiatry education [21]. Despite these challenges, the capacity of current computational technologies has reached a stage where its integration into psychiatric practice is not just feasible but urgently needed.
Computational psychiatry in practice: applications to specific disorders
Computational psychiatry has shown significant potential in modeling and the understanding of various psychiatric disorders. The application of computational methods has been explored in the context of schizophrenia, attention-deficit/hyperactivity disorder, autism spectrum disorder, anxiety disorders, obsessive-compulsive disorder, and substance use disorders [35–41].
In schizophrenia, the ‘Jumping-to-Conclusions’ bias, a tendency to make decisions based on insufficient evidence, has been modeled using Bayesian principles [35]. Similarly, the disruption of reward prediction errors in psychosis has been linked to the substantia nigra/ventral tegmental area [36]. In the context of negative symptoms, the failure to represent the expected reward value of actions has been explored using computational models [37].
In autism spectrum disorder, predictive coding theories have been used to explain the social deficits observed in these individuals [42]. Theories of anhedonia, a core symptom of depression, have been mapped onto reinforcement learning models [39].
In obsessive-compulsive disorder, specific frontostriatal circuits have been identified that are associated with impaired cognitive flexibility and goal-directed planning [43]. The tendency towards habitual behavior, a characteristic of compulsive disorders, has been modeled using computational methods [44].
In substance use disorders, the computational anatomy of addiction has been explored, with a focus on the role of uncertainty and anticipation in anxiety [45]. The application of CP in these disorders has not only provided a deeper understanding of their underlying mechanisms, but also opened up new avenues for their diagnosis and treatment [46, 47].
However, it is important to note that while these applications have provided valuable insights, they also highlight the complexity and heterogeneity of psychiatric disorders. Each disorder presents unique challenges that require tailored computational approaches.
Future directions and potential
Computational psychiatry is a rapidly evolving field with immense potential for future growth. The integration of computational technologies into psychiatric practice is not just feasible but urgently needed [48]. The development of more sophisticated mathematical models and computational simulations will continue to improve our understanding of mental disorders [49, 50].
The use of machine learning and big data in psychiatry is expected to revolutionize the way we predict and treat mental disorders [51]. Network analysis, for instance, offers an integrative approach to the understanding of the structure of psychopathology [52].
The field also faces challenges in terms of stigma and social adaptation, particularly among patients with first-episode schizophrenia [20]. The introduction of artificial companions to older adults with cognitive impairment, for example, may raise some concerns.
The future of CP also lies in interdisciplinary collaboration. The integration of neuroscience, psychiatry, and computer science will be crucial in advancing the field [34, 53]. The educational needs of mental health specialists will also need to be addressed to ensure the successful integration of computational methods into clinical practice [21–23]. Finally, the potential of computational psychiatry in genetic research cannot be ignored. The identification of risk loci with shared effects on major psychiatric disorders represents a significant breakthrough in the field [54].
In conclusion, while the future of CP is promising, it is also fraught with challenges.
DISCUSSION
Upon reviewing the literature concerned with the application of computational technologies in psychiatry, one may perceive an apparent impedance in its integration into practical healthcare. Despite more than a decade since the first mention of computational psychiatry in various publications [1], substantial changes in the field remain minimal. Nonetheless, the advancement of CP heavily relies on the synergy between computational scientists, neuroscientists, and clinicians. This interdisciplinary collaboration is essential to develop a comprehensive understanding of mental disorders and improve diagnostic accuracy, as well as to identify novel therapeutic targets and predict individual treatment responses. This potential of computational technologies in psychiatry has been recognized since the pioneering work of Hedlund et al. (1985) [34], who were among the first to shed light on both the potential and challenges associated with this integration.
Reflecting on the evolution of CP, it’s important to acknowledge the revolutionary shift that has occurred in the field. The advent of advanced computational tools and the increasing acceptance of technology in research have significantly expanded the capabilities of CP. This shift has not only enabled researchers to explore new avenues, but also to revisit existing concepts with a fresh perspective. Despite its 30 years of progress, there is still a palpable misunderstanding within both the literature and professional communities about these technologies. In particular, the tiptoeing around the utilization of computers by specialists persist. The recent integration of machine learning and AI into computational psychiatry has only served to intensify this sense of potential and novelty, offering unparalleled means to dissect complex psychiatric data. However, this area of scientific knowledge currently faces limitations as regards its development. Revisiting the key points discussed in the results section, it’s clear that the field of CP is marked by its interdisciplinary nature, the recognition and growth it has received, and its application to specific psychiatric disorders. Each of these aspects presents unique challenges but also hints at potential future directions for the field. The discussion of these key points in light of the extant literature not only provides a comprehensive overview of the current state of CP, but also sets the stage for future research.
Computational psychiatry has the potential to transform mental health care, laying the groundwork for personalized treatment approaches. The field of psychiatry, unfortunately, has been stigmatized due to limited understanding about the etiology of mental disorders, as well as misunderstandings related to the use of mathematical models. For instance, models that calculate probability values, such as risk degrees, can be misconstrued. When a personal data leak occurs or the essence of risks and probabilities is misunderstood, the risk of a mental disorder might be equated with a diagnosis, potentially leading to further stigmatization [30–32, 55]. This lack of comprehensive knowledge is one of the factors that fuel prejudice. Addressing this, CP strives to construct more intricate models of mental disorders [53]. This process requires the integration of a multitude of data sources, including neuroimaging [48], genetics [54], and behavioral data [1], and necessitates examining these data at different levels of analysis, from the molecular to the cellular and systems level [23]. This multi-modal and multi-level approach empowers researchers to untangle the complex interactions between the genetic [24], environmental [25], and neurobiological factors [26] that contribute to the onset and progression of psychiatric disorders. Importantly, this approach also facilitates the identification of biomarkers and endophenotypes [27], which can serve as essential tools for early diagnosis, prognosis, and the deployment of targeted interventions.
Ensuring the validity and reliability of computational models is crucial for their successful application in clinical practice. The discussion can emphasize the importance of rigorous model validation and evaluation techniques, which can help determine the accuracy and generalizability of these models across diverse patient populations. Access to large-scale, high-quality datasets is vital in this process, as it enables researchers to thoroughly test and refine their models based on real-world data. Encouraging the sharing of data and resources among researchers can facilitate model validation and promote reproducibility in CP.
The application of computational models in clinical decision-making raises several ethical concerns that need to be addressed. These include the potential for stigmatization or discrimination against certain patient groups, breaches of privacy, and misuse of sensitive patient data. It’s crucial to develop ethical guidelines and best practices to ensure that computational psychiatry adheres to the highest standards of patient care and confidentiality. Addressing these concerns is key for building trust among patients and clinicians and fostering the responsible growth of the field.
Three major ethical concerns emerge within the realm of computational methods in psychiatry, pertaining to screening, diagnosis, monitoring of conditions, and recommendations for therapy and rehabilitation. First, the security of patients’ personal data is a significant issue, albeit not unique to CP, as it extends to all digital workflows [30, 31]. Second, the potential stigmatization of patients is a common concern across the psychiatric field, where computational methods might inadvertently reinforce stereotypes or misconceptions [32, 55]. Finally, the misuse of sensitive information, which is closely related to the first challenge, necessitates stringent measures to ensure data privacy and integrity. These ethical considerations require thoughtful attention and the development of guidelines and best practices to foster responsible conduct in CP and safeguard patients’ rights and welfare.
The integration of CP into practical health care demands specialized education and training programs. That being said, it should be noted that in some countries psychiatrists still harbor concerns about the use of computers by professionals, including the use of modern technology in psychiatry training [23]. Meanwhile, more and more work is devoted to the reflection on the use of CP and digital methods in the education of psychiatrists [22, 56], noting both the possible advantages of this approach and its limitations, primarily ethical ones. The research, in the meantime, shows a high level of interest and demand in young psychiatrists for education in psychiatry, including scientific training [57], which may indirectly indicate the potential success in targeting educational programs in CP, specifically for this professional group. Education and training programs on CP must foster interdisciplinary collaboration, ensuring that specialists from various fields can communicate effectively and understand the common language of computational models and tools. Special emphasis should be placed on training clinicians to comprehend the applicability limits of AI-based models, integrating these tools into existing practices with consideration of data security measures and legal aspects [22]. Moreover, it’s essential to develop educational programs for patients to demystify the capabilities and limitations of computational psychiatry. This comprehensive educational approach will not only bridge the gap between computational scientists, neuroscientists, clinicians, and patients, but also pave the way for a more coherent and effective application of CP in mental health care.
Furthermore, enhancing the interpretability of models by making them more transparent and biologically plausible can foster their widespread adoption and improve their clinical utility. This emphasis on transparency and plausibility not only augments understanding, but can also contribute to a reduction in the stigmatization of computational psychiatry and its associated technologies.
It is important to also acknowledge the limitations and challenges inherent in CP, such as the need for more biologically plausible models, generalizability across diverse patient populations, and the integration of different levels of analysis. By identifying these limitations, the discussion can outline potential future directions for the field, such as refining existing models, exploring novel computational approaches, and fostering interdisciplinary collaboration. Addressing these challenges will be essential for the continued growth and success of CP in improving mental health care.
The main limitation of this article lies in its narrative review format, as opposed to a systematic review. While this approach allows for a broad overview of CP, it’s worth mentioning that potentially insightful articles that could have offered a more comprehensive understanding may not have been included in the search results. Therefore, the scope of our review may be inherently limited by the articles we have accessed. The breadth of the literature reviewed is also a major strength of the article. The authors hope that the literature review presented will generate interest in CP among psychiatrists, which in turn could lead to an increase in the number of studies in this field, as well as a willingness from professionals to use CP methodology in their work and clinical practice, which will be an example of the practical application of the scientific work done by the authors.
CONCLUSION
The field of computational psychiatry is a rapidly evolving discipline that integrates computational modeling, empirical data, and theoretical insights from various fields such as psychology, neuroscience, computer science, and mathematics. It aims to better understand psychiatric disorders and their underlying mechanisms. This interdisciplinary approach has led to significant advances in the field, including the development of novel diagnostic and therapeutic tools. However, the broad scope of CP also presents several challenges. These include the need for rigorous ethical guidelines to govern the use of computational models in psychiatric research and practice. The integration of computational methods into psychiatric research also requires a high degree of interdisciplinary collaboration, which can be challenging to achieve in practice.
Despite these challenges, the field of CP has seen significant growth and recognition over the past decade. This growth is evident in the increasing number of publications on the topic and the expanding range of psychiatric disorders to which computational methods are being applied. The application of computational methods to specific psychiatric disorders has yielded promising results. For example, computational models have been used to better understand the neurobiological mechanisms underlying disorders such as schizophrenia and depression. However, further research is needed to fully realize the potential of these methods in clinical practice.
Looking forward, the field of CP holds significant potential for advancing our understanding of psychiatric disorders and improving patient care. However, realizing this potential will require continued interdisciplinary collaboration, rigorous ethical oversight, and ongoing research to refine and validate computational models. While computational psychiatry is a promising field, it is also a complex one, with many challenges to overcome. However, with continued research, collaboration, and ethical oversight, it has the potential to significantly advance our understanding of psychiatric disorders and improve patient care.