Depression is one of the most common, disabling, and lethal (e.g., suicide) forms of psychopathology [Kessler, 2003; Whiteford, 2010]. Nearly 300 million people struggle with depression worldwide, and it is the leading cause of disability for people ages 15–44 [World Health Organization, 2017]. Unfortunately, most people with depression do not receive the treatment they need [Kessler, 2003; Kohn, 2004]. There are several reasons for the treatment gap, including poor case identification and limited access to mental health services. Further, when services are available, the treatments offered are typically not supported by scientific evidence [Baker, 2008; Gyani]. Many mental health professionals are not trained in empirically supported treatments (e.g., due to weak graduate program accreditation standards and/or a lack of national licensing requirements) and are skeptical about their usefulness [Baker, 2008]. This is a problem because, on average, empirically supported treatments are more effective than non-empirically supported treatments and thus, may decrease suffering and save patients money (that would have been used on sub-optimal treatment strategies). This does not mean that empirically supported treatments are always successful or that they will work for everyone; but, given a choice between
a treatment that helps 50% of people on average versus a treatment that helps 20% of people on average, which option would you prefer?
The purpose of this article is to provide a free and easy to use primer on one empirically supported treatment for depression ― Cognitive Behavioral Therapy (CBT). We discuss why CBT should be the first-line treatment for depression, provide a basic overview of the theoretical foundation of the treatment and how to conduct it, link to an open access workbook [11; https://osf.io/7ekz8/] that can supplement in-person therapy, and provide a reading list for further education (see Table).
Why Choose Cognitive Behavioral Therapy (CBT)?
There are a number of empirically supported treatments for depression, including CBT, cognitive therapy, behavior therapy, interpersonal therapy, and medication. Given these options, why choose CBT[Abramson, 1989] as the initial treatment? The first reason is that CBT is the most studied form of psychotherapy [Beck, 2005; Lorenzo-Luaces, 2018]; there are hundreds of studies testing the efficacy of CBT, and this work consistently finds that CBT for depression is as effective, or more effective, as all other therapies [e.g., 15]. Second, CBT is based on a well-articulated and empirically supported theory of cognition and depression [Abramson, 1989; Beck, 1967]. Third, research shows that the scientific results (from randomized controlled trials) generalize to real-world practice [Persons, 1999; von Brachel, 2019]. Finally, many of the basic treatment strategies used in CBT for depression can also be applied to other forms of psychopathology (e.g., anxiety disorders).
That said, even the best treatments do not work for everyone. The primary argument for using CBT is one of probabilities. The question to ask is ― given a person with depression, which treatment gives him or her the greatest probability of getting better right now? In other words, if you had to “bet” on a treatment working, which treatment would you pick? Our answer is CBT because it has the greatest level of empirical support, is as effective as all other treatments, including medication [Hollon], and is derived from basic cognitive research on appraisal and attribution theory. CBT gives a patient their greatest initial probability for improvement. If CBT does not work, which may very well be the case [Lorenzo-Luaces, 2022], then it is time to try another empirically supported treatment.
Theoretical Background
Arguably, the most consistent and robust predictor of depression is major life stress [Monroe]. Upwards of 80% of people with depression report experiencing a major life stressor prior to the start of their depressive episode [Mazure, 1998]. However, most people who experience a major stressor will not develop depression. Thus, given the same stressful life event, why is it that one person will develop depression and another will not? According to the cognitive theories of depression [Abramson, 1989; Beck, 1967], the answer to this question depends on whether or not the person possesses a cognitive vulnerability.
Cognitive vulnerability refers to the tendency of a person to generate overly negative inferences about the cause, consequences, and self-worth implications of stressful life events. Specifically, when faced with a stressful life event, an individual who has a cognitive vulnerability is likely to: (a) attribute the event to stable and global causes; (b) view the event as likely to lead to other negative consequences; and (c) construe the event as implying that he or she is unworthy or a failure. Individuals who generate these negative inferences are hypothesized to be at heightened risk for depression. There is strong empirical support for the cognitive vulnerability hypothesis as research has consistently shown that those who report high levels of cognitive vulnerability are at greater risk for developing depressive symptoms and depressive disorders during times of stress than those who generate more adaptive inferences (i.e., exhibit low levels of cognitive vulnerability [Haeffel, 2008; Nolen-Hoeksema, 2008]). Given this empirical work, it is not surprising that many treatments for depression are focused on changing cognitive vulnerability. The gold standard of which is CBT [Lorenzo-Luaces, 2018].
Treatment Basics
CBT is a collaborative, structured, and goal-oriented therapy that can be conducted individually or in groups. It uses both cognitive and behavioral strategies to change cognitive vulnerability and other maladaptive thinking patterns. Treatment typically consists of 12–20 hour-long sessions, but there is no strict limit on the number of sessions. Research suggests that twice-weekly sessions may be more effective than once-weekly sessions [Bruijniks]. Further, when CBT is effective, large and sustainable treatment gains are often reported as early as the fifth session [Lorenzo-Luaces, 2022; Shalom, 2020].
The overarching goal of the treatment is for the client to understand how one’s thoughts influence one’s mood. The client then learns specific strategies to change the negative patterns of thinking that maintain their depression (a process called “cognitive restructuring”). Throughout therapy, four points should be kept in mind:
1) CBT is not “positive thinking” therapy; the purpose is to teach the client more “realistic” thinking. It is not about turning lemons into lemonade but rather recognizing that the lemons may not be quite as terrible as believed;
2) CBT should be carried out within the context of a strong collaborative working alliance (which is necessary, but not sufficient, for successful treatment);
3) homework is a fundamental component of CBT. According to Dr. Judith Beck [Beck, 2021, p. 1], “We tell our patients that it is not enough to come to therapy and talk for 50 minutes a week. The way to get better is to make small changes in their thinking and behavior every day”;
4) therapists should administer measures of depressive symptoms (e.g., Patient Health Questionnaire (https://www.hrsa.gov/behavioral-health/patient-health-questionnaire-phq-screeners) or Beck Depression Inventory) weekly to track patient progress as symptom monitoring (by patient and clinician) improves therapy outcomes [Goodson, 2017]. Therapists should also routinely evaluate suicidal risk and substance use.
Session 1: Intake Interview
The first session is dedicated to proper diagnosis, case conceptualization, and establishing rapport. We recommend the therapist use a structured interview such as the Structured Clinical Interview for DSM Diagnoses (SCID) for diagnostic purposes as it reduces bias and increases reliability [Osório, 2019]. We acknowledge that conducting a full SCID is not feasible given time constraints, so the therapist should administer the sections that apply to the client (e.g., the most likely diagnoses). The therapist should also evaluate suicidal risk, psychosocial history, and medical history.
Session 2: Socialization to Treatment
The second session is dedicated to a review of the diagnosis, socialization to treatment, and treatment goals. The client is informed of their diagnosis of Major Depressive Disorder (or other depressive disorder) and that it can be treated with a gold standard intervention called Cognitive Behavioral Therapy (CBT for short). The therapist should try to instill hope that therapy will be successful. The therapist should also highlight the collaborative nature of the treatment and the use of homework (also called “action plans”) between sessions [Yew, 2021].
The client is then taught the general cognitive model (see Figure). Specifically, the client learns to differentiate thoughts and moods. They are then taught that when negative thoughts are changed, then negative moods, behaviors, and even neurochemistry and brain activation patterns also change. Finally, the therapist and client create a list of treatment goals.
Sessions 3–10: Cognitive Restructuring, Experiments, and Behavioral Activation
The majority of sessions are focused on changing negative patterns of thinking. As
a reminder, clients should always complete a symptom measure at the start of each session. Further, each session should begin by creating an agenda that includes a discussion of events since the last session, a review of homework, goal(s) for the current session, and skill acquisition.
Clients first learn to identify and rate their moods. As clients become adept at monitoring their moods, they are then taught to identify the negative automatic thoughts that precede and accompany depressed moods. These negative cognitions become the target for cognitive restructuring. Throughout this learning process, clients also may begin to identify situational factors that affect their moods (e.g., depression is worst in the morning).
Cognitive restructuring is a deliberate and effortful process by which clients evaluate and challenge the veracity of their negative thoughts. It is typically accomplished with Socratic-style questioning from the therapist (e.g., would your friend agree with that?) as well as the use of thought and behavior experiments. Perhaps the most common technique is for the client to serve as a “judge” for their thoughts; they write down the evidence “for” and “against” negative thoughts using a thought record worksheet. After considering all the evidence, they then try to generate more realistic or less extreme cognitive responses. These skills are practiced both in-session and outside of session via homework. Behavioral experiments are also used to test the accuracy of negative thoughts and beliefs. For example, a client may have thought, “no one wants to spend time with me.” The client could then test this thought by asking a friend to get coffee. It may be helpful to think about cognitive restructuring as learning a second language [Haeffel, 2019]; both take time, practice, and overcoming highly engrained patterns of thinking.
In addition to cognitive restructuring, clients should engage in behavioral activation. For example, it is useful to create a weekly activity schedule to increase goal-directed behaviors (e.g., go for a 15-minute walk or visit a friend). It is important to pursue activities from which the client not only derives pleasure but also can experience a sense of accomplishment. Thus, small attainable activities should be the focus.
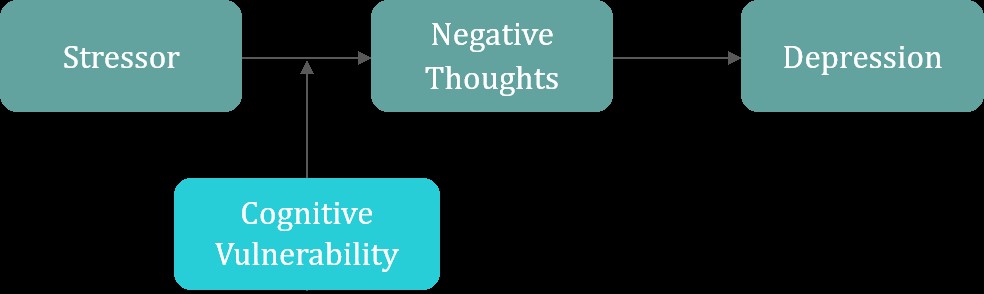
Figure. Basic Cognitive Model of Depression
Sessions 11–12: Consolidating Treatment Gains and Relapse Prevention
The final sessions are dedicated to consolidating the skills the client has learned. The patient should be well versed in the cognitive model of depression, competent at identifying automatic thoughts, cognitive restructuring, and behavioral activation. The patient should continue to do homework and practice their cognitive skills while both the client and therapist try to anticipate challenges that may arise after therapy termination.
Materials for Further Education
Cognitive Skills Workbook. We created a cognitive skills workbook that can supplement in-person CBT [Haeffel, 2010]. It can be downloaded here: https://osf.io/7ekz8/. This workbook provides psychoeducational activities (e.g., thought records) that can be used in sessions or as homework. This is not meant to be a standalone intervention, and its efficacy was only tested in relatively healthy American college students [Haeffel, 2010].
Reading List
Table
Articles that provide more in-depth analyses of CBT, including how to conduct it and its efficacy
|
Manuals and Guides |
|
Beck, J.S. (2011, November 17). The How and Why of Cognitive Behavior Therapy. https://www.huffpost.com/entry/the-how-and-why-of-cognit_b_628131 |
|
Beck, J.S. (2011, November 17). Cognitive Behavior Therapy: Myths and Reality. https://www.huffpost.com/entry/cognitive-behavior-therap_b_638396 |
|
Leahy, R.L., Holland, S.J. F., & McGinn, L.K. (2012). Treatment Plans and Interventions |
|
Padesky, C.A. (2020). The Clinician's Guide to CBT Using Mind Over Mood. |
|
The Psych Show. (2019, January 22). 5 signs you’re getting bad cognitive behavioral therapy [Video]. YouTube. URL: https://www.youtube.com/watch?v=jqctZgdWtok |
|
Young, J.E., Rygh, J.L., Weinberger, A.D., & Beck, A.T. (2014). Cognitive therapy for depression. In D.H. Barlow (Ed.), Clinical Handbook of Psychological Disorders: |
|
Theory and Evidence |
|
Beck, A.T. (2005). The current state of cognitive therapy: a 40-year retrospective. Archives of General Psychiatry, 62, 953–959. DOI: 10.1001/archpsyc.62.9.953 |
|
Beck, A.T. & Haigh, E.A. (2014). Advances in cognitive theory and therapy: |
|
Clark, D.M. (2018). Realizing the mass public benefit of evidence-based psychological therapies: The IAPT Program. Annual Review of Clinical Psychology, vol. 14, |
|
Hollon, S.D. (2020). Is cognitive therapy enduring or antidepressant medications iatrogenic? Depression as an evolved adaptation. American Psychologist, vol. 75, |
|
Hollon, S.D., DeRubeis, R.J., Andrews, P.W., & Thomson, J.A. (2021). Cognitive therapy |
|
Lorenzo-Luaces, L., German, R.E., & DeRubeis, R.J. (2015). It's complicated: The relation between cognitive change procedures, cognitive change, and symptom change in cognitive therapy for depression. Clinical Psychology Review, vol. 41, pp. 3–15. DOI: 10.1016/j.cpr.2014.12.003 |
|
Strunk, D.R., DeRubeis, R.J., Chiu, A.W., & Alvarez, J. (2007). Patients' competence |
|
Yew, R.Y., Dobson, K.S., Zyphur, M., & Kazantzis, N. (2021). Mediators and moderators |
Notes. To obtain copies of peer reviewed articles behind paywalls, please email the corresponding author of the article or you can email the corresponding author of this article.
Conclusion
When a patient presents with depression, which treatment should a therapist try first? We argue that it is best to start with Cognitive Behavioral Therapy (CBT). It is the most studied form of psychotherapy, has a strong theoretical basis, can be implemented by therapists of varying experience levels, and is as effective or more effective than existing treatments, including medication. CBT may not work for every client, but it is the best place to start.
[Abramson, 1989] We define “CBT” as a treatment protocol that combines cognitive and behavioral techniques to try to alter maladaptive thinking patters (e.g., cognitive vulnerability; Lorenzo-Luaces and colleagues, 2016).