INTRODUCTION
The traditional approach to achieving high adherence to treatment in patients with severe mental disorders is the widest possible use of depot antipsychotics. However, despite the general consensus on the described strategy,1 the practice of using prolonged-release antipsychotics in various healthcare institutions remains inconsistent and, even taking into account the greater cost, is unreasonably limited.2
Among the barrier factors for the widespread use of depot drugs in clinical work are organizational factors (a limited number of drugs paid for from insurance funds due to a high cost for depot antipsychotics), the doctors` attitude (difficulties in dose control, subjective perception of the appointment as coercion of the patient, established clinical practice), or factors related to the patient, such as a fear of painful injections, lack of information or perception of depot therapy as a coercive measure.3 At the same time, an analysis of the frequency of prolonged-release antipsychotics use indicates their predominant prescription in situations of clinical uncertainty: among 37.8% of patients with polypharmacy,4 as well as among those with increased aggressiveness5 and those who rarely seek in-patient care.6 At the same time, the question remains unclear whether such categories of patients benefit the most from the depot therapy. On the contrary, some clinical recommendations indicate the validity of using depot drugs not only for the treatment of severe patients, but also as a choice for routine anti-relapse therapy.7
It is noteworthy that psychiatrists themselves are often biased towards prolonged-release antipsychotics, and in a hypothetical situation of their own treatment they would prefer taking oral drugs.8 This prejudice associated with changing patterns of behavior is believed to be one of the key markers of the stigmatization process.9 Stereotyping attitudes towards patients and strategies for choosing drug therapy can determine cognitive biases. Then, in order to increase adherence to treatment, depot therapy is prescribed algorithmically and without considering recommendations on the need to combine prolonged-release antipsychotics with psychoeducation programs to achieve the desired level of compliance.10
There is solid evidence that different categories of patients demonstrate significantly different rates of treatment adherence, even with depot antipsychotics, depending on their motivation for treatment and attitude to the disease.11 At the same time, in addition to the patient’s own motivation for treatment, the perceived external pressure from the patient’s environment is an independent factor in increasing involvement in the therapeutic process, acting along with the factors of distress and insight on the disease.12
From this review of the literature, it follows that the task of forming a high adherence to antipsychotic therapy in severe mental disorders is intractable in the case of a mechanistic prescription of depot drugs to the most severe patients. On the contrary, the benefits of therapy with prolonged-release antipsychotics could be available to a larger number of patients through the development of personalized rehabilitation programs that include, along with the individualized selection of medical therapy, taking into account the socio-psychological conditions of a mental disorder development and the patient’s own motives for therapy.
The purpose of the study is a differentiated description of the role of clinical and socio-psychological factors involved in the formation of different levels of in-patient engagement in the treatment process. The hypothesis of the study was based on the assumption that the level of involvement of patients with mental disorders in therapy is available for instrumental analysis and can be increased through rehabilitation strategies addressed to morbid (biological), motivational (psychological), and socio-behavioral factors specific to different types of patients. The implementation of the study was carried out through a sequential completion of tasks:
1) verification, based on the objectively observed behavior of patients during treatment and their therapeutic alliance, of the original cluster model of involvement in the treatment process, based on an instrumental assessment of therapeutic motivation and the structure of compliance
2) description of targeted strategies to increase adherence to treatment, depending on the main clinical, psychological and behavioral parameters: severity of symptoms, characteristics of the course of the disorder and attitude to the disease, and the therapeutic alliance, in each of the selected types of patients.
METHODS
A sample of 91 patients of the V.M. Bekhterev National Research Medical Center for Psychiatry and Neurology was studied, clinical and experimental psychological data were subjected to secondary analysis in February 2020, after identifying the typology of patients based on their motivation for treatment and profile of drug compliance. A detailed description of the examined respondents is presented in Table 1. The study protocol was implemented in accordance with the principles of the Declaration of Helsinki, GCP and approved at a meeting of the Independent Ethics Committee at the V.M. Bekhterev National Research Medical Center for Psychiatry and Neurology No. EK-I-105/18 (25.09.2018).
Table 1. Sociological and clinical features of patients after clusterization
|
Cluster 1 N=29 |
Cluster 2 N=23 |
Cluster 3 N=39 |
p-level of differences |
||
|
Sex |
Male |
15 |
8 |
11 |
≥0.05 |
|
Female |
14 |
15 |
28 |
||
|
Mean age, years, M [S.D.] |
30.7 [9.8] |
36.1 [12.5] |
35.1 [13.2] |
≥0.05 |
|
|
Occupation |
employed |
5 |
9 |
20 |
p=0.046 |
|
unemployed |
23 |
12 |
17 |
||
|
disability pension |
1 |
2 |
2 |
||
|
Marital status |
married |
9 |
11 |
10 |
≥0.05 |
|
single |
20 |
12 |
29 |
||
|
Education |
primary |
11 |
4 |
8 |
≥0.05 |
|
secondary |
8 |
7 |
5 |
||
|
higher |
10 |
12 |
26 |
||
|
Diagnosis (ICD-10) |
F2 |
24 |
15 |
30 |
≥0.05 |
|
F3 |
2 |
4 |
2 |
||
|
F4+F6 |
1 |
3 |
5 |
||
|
F0 |
2 |
1 |
2 |
||
|
Illness duration, years, M [S.D.] |
8.9 [9.5] |
10.4 [11.0] |
8.1 [8.0] |
≥0.05 |
|
|
Inter hospitalization rate, months, M [S.D.] |
34.3 [27.5] |
25.7 [21.6] |
≥0.05 |
||
|
BPRS (positive symptoms) |
≥60 points |
12 |
6 |
7 |
≥0.05 |
|
40-60 points |
14 |
12 |
24 |
||
|
≤40 points |
3 |
5 |
8 |
||
|
SANS (negative symptoms) |
≥60 points |
13 |
5 |
5 |
p=0.004 |
|
30-60 points |
13 |
8 |
14 |
||
|
≤30 points |
3 |
10 |
20 |
||
|
GAF (global functioning) |
≤40 points |
13 |
6 |
4 |
p=0.015 |
|
40-60 points |
13 |
11 |
28 |
||
|
≥60 points |
3 |
6 |
7 |
||
To identify the reasons for the motivation of patients included in the study, as well as to operationalize their drug compliance, the original psychometric instruments were used. The Treatment Motivation Assessment Questionnaire (TMAQ) was applied, based on the Treatment Motivation Scale developed in the Department of Integrative Pharmaco-Psychotherapy.13 Therapeutic motivation is described quantitatively – through the total indicator of its intensity, and also qualitatively – when comparing the parameters of individual sections with those standardized for six levels or four factors of the questionnaire. It has demonstrated good internal consistency (Cronbach’s alpha 0.842), and its external as well as meaningful validity has been established previously.13,14
To assess the multifactorial nature of patient compliance, the Medication Compliance Scale (MCS)15 was used, which is answered by a doctor based on complete clinical information and medical history of the patient. Individual MCS items include the study of the patient’s clinical condition according to the Brief Psychiatric Rating Scale (BPRS),16 the Negative Symptom Rating Scale (SANS),17 and the Global Assessment of Functioning (GAF).18 In addition to the original psychometric instruments, the Internalized Stigma of Mental Illness (ISMI) scale19 and the Perceived Discrimination and Devaluation Scale (PDD)20 were used.
The data obtained were statistically analysed using the SPSS 16.0 software package. The principal component method with varimax rotation was used to factorize the data. The k-means cluster analysis was used. Analysis of variance was performed using ANOVA and the Student’s t-test for parametric data, Kruskal–Wallis H-criterion and Mann–Whitney U-criterion for nonparametric data and Pearson Chi-square for rated values. The data distribution was assessed using the Kolmogorov-Smirnov z-criterion. For descriptive statistics of revealed significant differences, we used the calculation of the size of effects according to the Cohen’s d and Cramer’s V criteria.
Study procedures
Enrolment in the study was carried out after obtaining voluntary informed consent. The inclusion criteria were:
1) being in in-patient treatment in the department of integrative pharmaco-psychotherapy of patients with mental disorders, 2) readiness and ability to undergo psychometric examination in accordance with the protocol, and 3) fluency in Russian. Noninclusion criteria: the severity of the positive symptoms or cognitive impairments, which determines the patient’s inability to correctly answer the questions of the original psychometric instruments. The exclusion criterion was the withdrawal of consent to participate at any stage of the study.
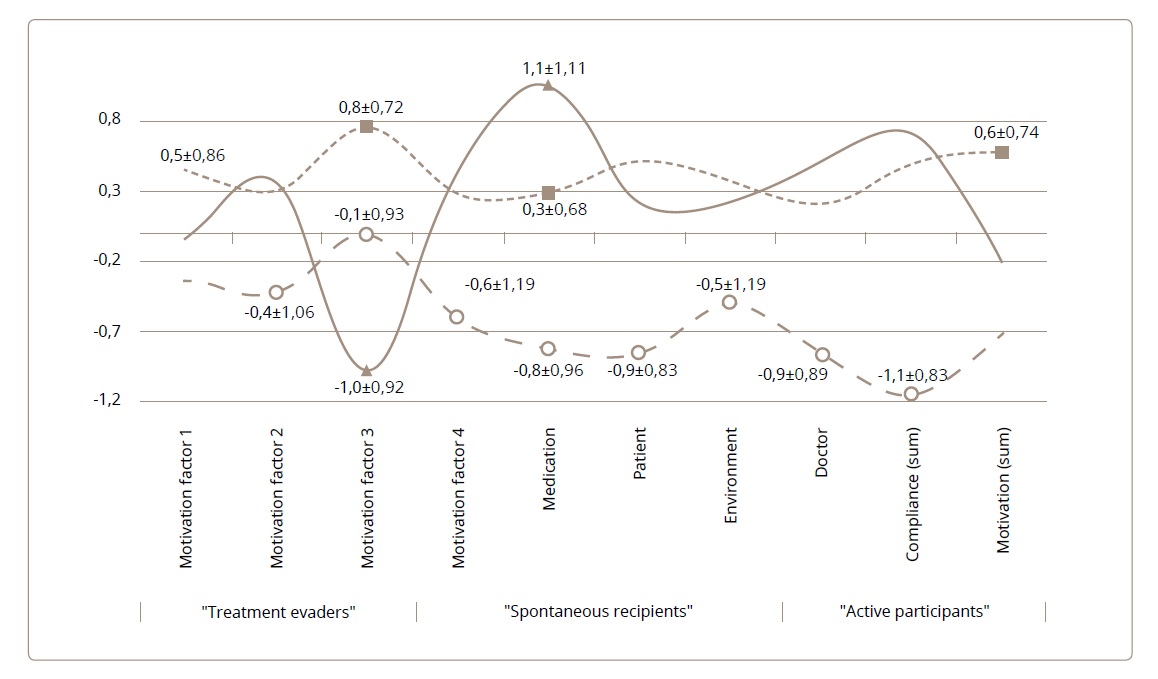
The most typical options for the involvement of in-patients in the treatment process were established in the cluster analysis of psychometric data: standardized indicators of the compliance scale subscales and four factors of the motivation assessment questionnaire.21 The selected groups of patients had the most similar structures of motivation for treatment and drug compliance within the cluster, but they differed maximally when compared with each other (Figure 1).
Figure 1. Typology of patients depending on the prevailing structure of treatment motivation and the corresponding profile of medication compliance (means and standard deviations of questionnaires standardized indices).
Footnote. Parameters of the Treatment motivation assessment questionnaire (TMAQ): factor 1 – the psychoeducative component of the internal disease picture, factor 2 – the insight into the necessity of the treatment, factor 3 – the insight into the psychological mechanism of the morbid social maladjustment, factor 4 – the willingness to an active participation in the treatment process, motivation – the sum total of TMAQ. Subscales of Medication Compliance Scale (MCS): medication – the attitude to medication, patient – factors referring to the patient, environment – factors referring to the environment of the patient, doctor – factors referring to the therapist, compliance – the sum total of the MCS. Marked standardized indices with significant intergroup differences, Cohen's d≥0.74; p≤0.05.
RESULTS
Patient clusters, differing in the degree of involvement in therapy, were numerically comparable (Table 1) and did not differ in the main socio-demographic and clinical characteristics (gender, age, education, marital status and children, nosology, duration of the disease, frequency of hospitalizations, severity of productive symptoms), as well as the frequency of taking antipsychotics of the 1st or the 2nd generations, antidepressants and mood stabilizers.
The fundamental difference was in the behavior of patients assigned to different clusters during drug treatment and in their therapeutic alliance (Table 2).
Table 2. Differences in the prevalence of compliance violation history between groups of patients after clustering
|
Predominant behavioral pattern in medication compliance scale |
Behavior occurrence |
Criterion of differences |
||
|
Cluster 1 |
Cluster 2 |
Cluster 3 |
||
|
1.1 Behavior during medication |
||||
|
Evasion of medication intake |
3 |
0 |
0 |
p=0,0001; χ2=23.4, df=4, Cramer’s V=0.51 |
|
Externaly controlled drugs intake |
18 |
6 |
8 |
|
|
Self-controlled drugs intake |
8 |
17 |
31 |
|
|
1.5 Noncompliance history |
||||
|
Nonrecommended drugs intake |
5 |
1 |
2 |
p=0,002; χ2=24.1, df=8, Cramer’s V=0.52 |
|
Self-discontinuation of medication |
14 |
5 |
19 |
|
|
Irregular intake of medication |
4 |
0 |
2 |
|
|
Self-reduced dosage |
0 |
4 |
4 |
|
|
Absence of noncompliance |
3 |
13 |
12 |
|
|
4.1 Therapeutic alliance |
||||
|
Low |
15 |
0 |
1 |
p=0,0001; χ2=41.1, df=4, Cramer’s V=0.67 |
|
Medium |
13 |
12 |
28 |
|
|
High |
1 |
11 |
10 |
|
The proportion of patients in cluster 1 was overwhelming among respondents with a low therapeutic alliance (MCS 4.1). Often, they were unable to maintain drug compliance on their own. The adherence disorder for these “evading” patients was stable throughout the whole available medical history (MCS 1.5). Patients in this cluster included those with more frequent use of nonrecommended drugs and / or irregular use of recommended medications. The search for factors involved in the formation of low adherence to treatment in cluster 1 revealed the most pronounced morbid changes in this group of patients. They suffered from negative symptoms, and, compared to patients in cluster 3, were more socially maladjusted (Table 1).
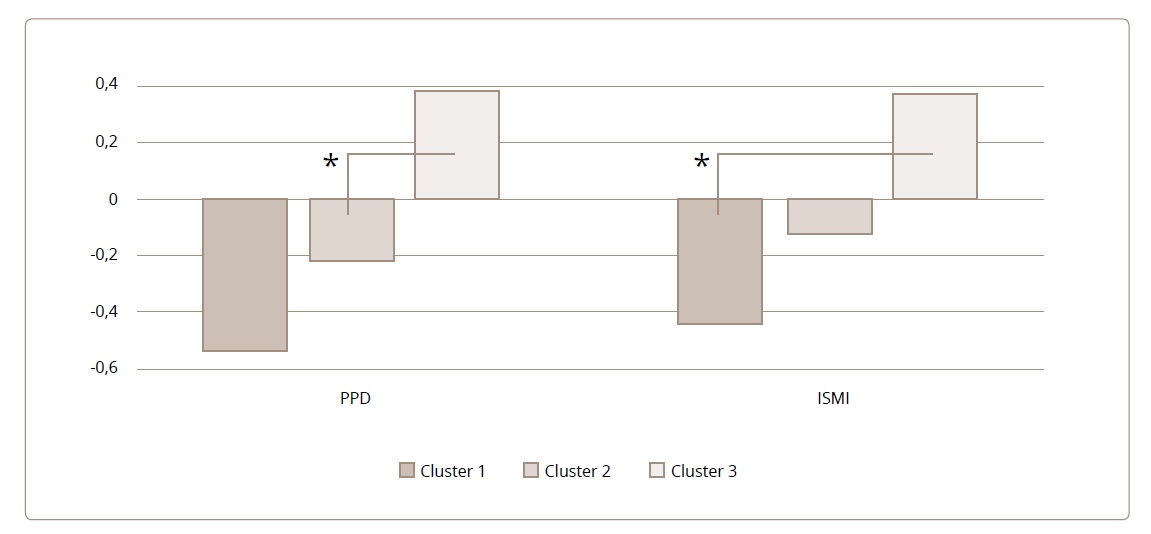
Cluster 2 included half of the subgroup of respondents with a high therapeutic alliance, as well as 19% of patients who needed external control of medication and 30% who were self-medicating at the time of the current hospitalization. Nevertheless, this cluster included the rarest history of drug compliance violations (Table 2). Interestingly, such “recipients of therapy” were more inclined to discriminate against other mentally ill patients than in cluster 3 (Figure 2).
Figure 2. Standardized scores for psychiatric stigmatization in patients from different clusters (means and standard deviations).
Footnote. PDD — Perceived Discrimination and Devaluation Scale (low scores reflect higher external stigmatization); ISMI — discrimination resistance subscale of Internalized Stigma of Mental Illness; Cluster 1 — patients «avoiding treatment»; Cluster 2 — «passive recipients» of treatment; Cluster 3 «active treatment participants». *p<0,05
In cluster 3, with the maximum indicators of the intensity of therapeutic motivation, the most common was the average level of therapeutic alliance and attitude to medication. Unexpectedly, this group included half of the patients who have arbitrarily discontinued drug therapy in the past. It is important to note separately that the respondents here were inclined to actively resist psychiatric stigmatization (Figure 2).
DISCUSSION
The study confirmed the hypothesis of the complex nature of the phenomenon of long-term adherence to drug therapy in psychiatric in-patients. The fact of a high intensity of motivation for treatment, without its nature assessment, does not allow for predicting a favourable attitude towards medication and a high therapeutic alliance in patients with severe mental disorders. The data obtained demonstrate that, in addition to the factor of insight into the disease described earlier in the literature,11 the processes of psychiatric stigmatization play a significant role in the formation of adherence to therapy in hospital patients with severe mental disorders.
Long-term adherence to antipsychotic therapy is critical for the decrease of productive symptoms and the prevention of maladjustment in schizophrenia patients.22 Based on the data of the analysed sample, it was revealed that among patients with impaired functioning, unfavourable social and labour status and the most pronounced negative symptoms, low drug compliance is associated with impaired motivation for treatment. Thus, the patients most in need of stable drug treatment did not have sufficient psychological resources to maintain a therapeutic alliance and adherence to treatment. The prevalence of the irregular use of drugs in such “difficult” patients determines the rationale that 32% of the examined patients should be treated with prolonged-release antipsychotics in combination with the active formation and maintenance of a therapeutic alliance, their family should be involved in psychoeducation and training in the supervision of the patient’s medication.
Only one fourth of the sample showed long-term adherence to therapy. Adherence was supported by a moderate intensity of motivation for treatment, which became an illustration of the applicability of the “law of optimum” in relation to therapeutic motivation in patients with severe mental disorders.23 However, patient compliance is not the only barrier to the use of long-acting antipsychotics. Since they discriminated against other psychiatric patients and showed a relative decrease in the motivation for treatment, it is legitimate to judge the limited self-identification of “recipients of therapy” as patients in need of psychiatric care. Thus, it is more important for this category of patients to prevent the formation of a semantic connection between the depot as a therapeutic option and the risk of limiting their freedom in choosing a treatment strategy, rather than ensuring the constant receipt of the antipsychotic in the form of a depot.
A significant (43%) part of the sample (highly functioning patients with no signs of severe abulia) were active in opposing discrimination. This is consistent with literature data on the multidimensional relationship between motivational processes, internal stigma, and disease outcome.24 Active and purposeful actions of patients within the therapeutic program are not only a reflection of their overall high level of functioning, but also an indirect effect of overcoming self-stigmatization affected by their involvement in the rehabilitation system. Probably, among the “active participants” of therapy, the motive of resistance to stigmatization had an expansive subjective interpretation in the form of distancing from the doctor (middle-level therapeutic alliance) and, thus, was associated with a medical history aggravated by therapy discontinuation. These findings highlight the potential for the increased use of long-acting antipsychotics also in patients who demonstrate an active stance during treatment, when combined with rehabilitation interventions aimed at correcting dysfunctional beliefs about illness and medication.
A potential limitation of the study is the nosological heterogeneity of the sample. However, a significant part of the social and psychological factors that determine involvement in the therapeutic process is the same in various mental disorders. Therefore, samples mixed by diagnosis are widely represented in studies addressed to the psychology of the treatment process.25,26 Our sample of patients reflects the naturalistic nosological profile of patients with mental disorders seeking for in-patient care. In addition, there were no statistically significant nosological differences between the identified clusters of patients with different levels of inclusion in therapy. Thus, the objective of the study did not depend on bias in the selection of patients.
CONCLUSION
Verification of the original cluster model has demonstrated the applicability of instrumental assessments of motivation to treatment and drug compliance to determine the types of treatment involvement of patients with mental disorders. Analysis of the differences between the identified clusters of “active participants”, “passive recipients” and patients that “avoided therapy” helps to objectively assess the multifactorial nature of patients’ behavior during the treatment process. The level of compliance of patients with severe mental disorders is mediated by the severity of negative symptoms and social maladjustment, various motivational and behavioral styles, and the intensity of psychiatric stigmatization. Taking these factors into account empirically determines the strategies for the personalized use of prolonged forms of antipsychotics when developing an individual treatment plan for psychiatric in-patients.