INTRODUCTION
Sri Lanka is an island nation in the Indian Ocean, separated from the Indian peninsular by the Palk Strait. It has a total land area of 65,610 km2 and the capital city is Colombo.1
A number of different ethnicities live together in the country with the majority being Sinhalese (74.9%) while Tamils, Muslims and other minorities make up the rest of the population.2 The mid-year population of Sri Lanka in 2019 was 21.803 million with an annual growth rate of 0.62%. There are 93.9 males for every 100 females and the median age of the population is 31 years.3 Sri Lanka has an ageing population, as in most other countries, with the Ageing Index (ratio of 60 years and over population to 0–14 year population) increasing from 18.8 percent in 1981 to 48.8 percent in 2019.3 The population density is 348 per km2 but over half of the population is concentrated in the Western, Central and Southern provinces, which when combined, cover less than a quarter of the total land area of the country.2
The World Bank has designated Sri Lanka a lower middle-income country. The total government health expenditure as a percentage of government expenditure in 2018 was 8.28%, which was above the average for South Asia (3.57%)4 and as a percentage of gross domestic product in 2018 was 1.54%, which was higher than the regional average (0.95%).5
THE HISTORY AND EVOLUTION OF HEALTH SYSTEMS IN SRI LANKA
The healthcare system in Sri Lanka has evolved over 2000 years and has been influenced by many intrinsic and extrinsic factors.
Even around 543BC, when Sri Lankan recorded history begins, there are records of a system of hospitals, environmental sanitation and other related services during the reigns of the ancient kings. Traditional medical practices were a confluence of native medicinal practices known as “Deshiya Chikitsa”, Ayurveda and Siddhi medicine (originating from India) and Arabic Unani medicine.6
Western medicine was introduced to Sri Lanka, then known as Ceylon, by the Portuguese who invaded the coastal areas of the country in 1505. The Portuguese and thereafter the Dutch, who displaced them, established a few hospitals in the coastal belt of Sri Lanka, mainly to treat their own soldiers. When the English invaded the country in 1876, bringing the entire nation under its rule in 1815, they further expanded the services which were already established. In 1859, the Civil Medical Department was created, which primarily provided services for the care of the sick, while a sanitary branch of the Civil Medical Department, which was responsible for environmental sanitation and prevention of communicable diseases, was established in 1915.7
Due to the influence of nationalist forces, Ceylon gained independence from British colonial rule in 1948, and in 1972 it became the Democratic Socialist Republic of Sri Lanka.8 After gaining independence, Sri Lanka offered free universal healthcare to its citizens and over the next 70 years the country has achieved a relatively good level of healthcare, despite being a lower middle-income country.9
Listed below in Table 1 are the key socioeconomic and health expenditure indicators, while Table 2 shows selected health outcome indicators for Sri Lanka and a few other selected countries in the region (Table 1 and Table 2).
Table 1. Key socioeconomic indicators and health expenditure of selected countries in the region
|
Country |
Sri Lanka |
Bangladesh |
India |
Pakistan |
Malaysia |
Thailand |
Vietnam |
|
Population in millions ( 2020) |
21.92 |
164.70 |
1380 |
220.90 |
32.36 |
69.80 |
97.34 |
|
GNI per capita, Atlas method, current US$ (2020) |
3721 |
2010 |
1900 |
1280 |
10580 |
7050 |
2660 |
|
CHE as a percentage of GDP (2018) |
3.8 |
2.3 |
3.5 |
3.2 |
3.8 |
3.8 |
5.9 |
|
CHE per capita Int $ (2018) |
516.9 |
109.6 |
275.1 |
178.2 |
1193.9 |
722.7 |
440.2 |
|
Domestic general government health expenditure as a percentage of CHE (2018) |
8.3 |
3 |
3.4 |
5.3 |
8.5 |
15 |
9.3 |
|
Literacy rate, adult total (% of people ages 15 and above) |
91.7 |
73.9 |
74.4 |
59.1 (2017) |
94.9 |
93.8 |
95 |
|
Rural population (% of total population) |
81.3 |
61.8 |
65.1 |
62.8 |
22.8 |
48.6 |
62.7 |
|
Hospital beds (per 1,000 people) 2017 |
4.2 |
0.8 (2016) |
0.5 |
0.6 |
1.9 |
- |
- |
|
Physicians (per 1,000 people) 2018 |
1.0 |
0.6 |
0.9 |
1.0 |
1.5 (2015) |
0.8 |
0.8 (2016) |
|
Nurses and midwives (per 1,000 people) 2018 |
2.2 |
0.4 |
1.7 |
0.7 |
3.5 (2017) |
2.8 |
1.4 (2016) |
GNI — Gross National Income; CHE — Current Health Expenditure, GDP; Gross Domestic Product; Int $ — International dollars
Source: World Bank Open Data | Data [Internet]. [cited 2021 Aug 19]. Available from: https://data.worldbank.org/
Table 2. Selected health outcome indicators of selected countries
|
Country |
Sri Lanka |
Bangladesh |
India |
Pakistan |
Malaysia |
Thailand |
Vietnam |
|
Life expectancy at birth, total (years) 2019 |
77.0 |
72.6 |
69.7 |
67.3 |
76.2 |
77.2 |
75.4 |
|
Maternal mortality ratio (modeled estimate, per 100,000 live births) 2017 |
36 |
173 |
145 |
140 |
29 |
37 |
43 |
|
Mortality rate, infant (per 1,000 live births) 2019 |
6.1 |
25.6 |
28.3 |
55.7 |
7.3 |
7.7 |
15.9 |
|
Mortality rate, under-5 (per 1,000) |
7.1 |
30.8 |
34.3 |
67.2 |
8.6 |
9.0 |
19.9 |
|
Human development Index 2020 (Rank) |
0.782 (72) |
0.632 (133) |
0.645 (131) |
0.557 (154) |
0.810 (62) |
0.777 (79) |
0.704 (117) |
Sources:
- World Bank Open Data | Data [Internet]. [cited 2021 Aug 19]. Available from: https://data.worldbank.org/
- Latest Human Development Index Ranking | Human Development Reports [Internet]. [cited 2021 Aug 19]. Available from: http://hdr.undp.org/en/content/latest-human-development-index-ranking
Currently allopathic medicine caters for the majority of the health needs of the people but this is heavily supplemented by Ayurvedic medicine, and to a lesser extent by Unani, Siddhi acupuncture and homeopathic systems. These traditional methods are practiced mostly in the private sector.9
ALLOPATHIC MEDICINE SYSTEM
This is delivered both by the government and the private providers and includes promotive, curative, preventive and rehabilitative services.11
The Ministry of Health (Central Government) is primarily responsible for the provision of comprehensive health services in the public sector and delivers its services through the Department of Health Services, headed by the Director General of Health Services.10
It is mainly responsible for setting policy guidelines, training health personnel, managing teaching and specialized medical institutions and the bulk purchase of medical requisites.
The establishment of provincial councils following the 13th amendment to the constitution in 1987 was a major reform, as it led to the devolution of the provision of healthcare to the provincial councils, which now have ultimate responsibility for the provision of healthcare in the provinces.10
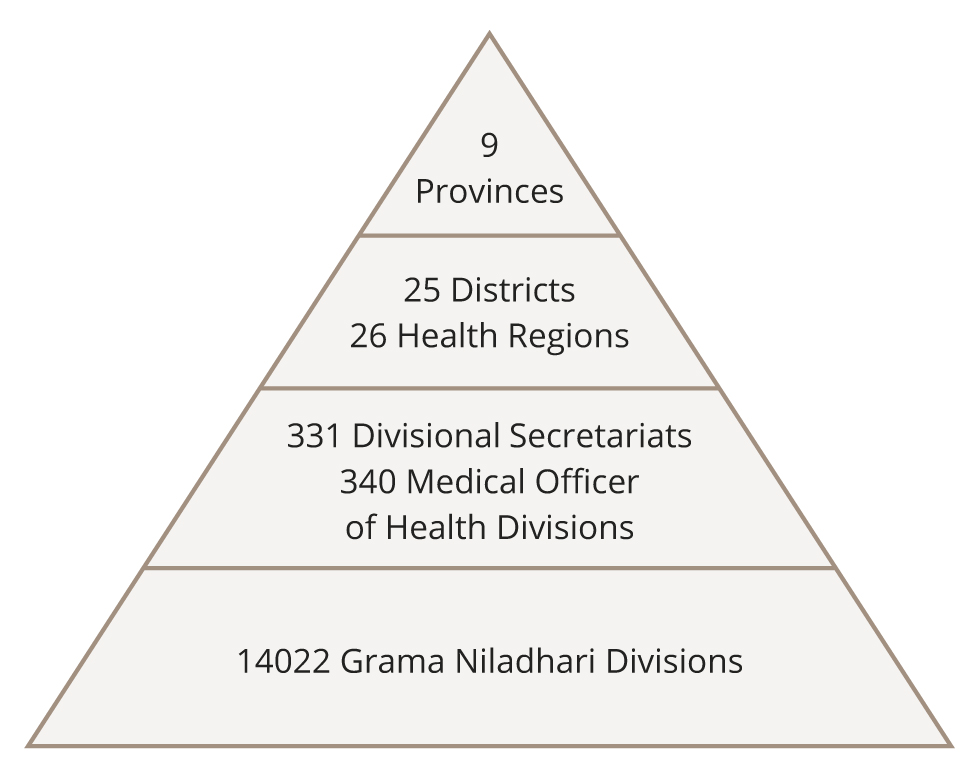
The provincial directors of health head up the administrative structure with the district directors of health for each district under them. Each district is then served by a defined number of medical officers of health (MOHs), who are responsible for a defined geographical area with a defined population. In each MOH area, services are provided by medical officers and several categories of field personnel, including public health nursing sisters, public health inspectors and public health midwives, who mainly focus on preventive aspects of healthcare delivery.10
Figure 1 shows the provincial administrative structure of governance in Sri Lanka (Figure 1).
Figure 1. Provincial administrative and health care structure. Reproduced with permission.
A cross section of the current status of the free health services in the public sector for 2019 is presented in Table 3.
Table 3. Selected statistics of public health sector in Sri Lanka
|
Medical Officers per 100,000 population |
93.5 |
|
Population per Medical Officer |
1,069.8 |
|
Dental Surgeons per 100,000 population |
7.2 |
|
Nurses per 100,000 population |
214.8 |
|
Supervising Public Health Midwives/Public Health Midwives per 100,000 population |
27.7 |
|
Number of hospitals |
643 |
|
Number of hospital beds |
86,589 |
|
Hospital beds per 1,000 population |
4.0 |
|
Number of Medical Officer of Health (MOH) Divisions |
356 |
Source: Ministry Of Health — Annual Health Statistics [Internet]. [cited 2021 Aug 19]. Available from: http://www.health.gov.lk/moh_final/english/public/elfinder/files/publications/AHB/AHS%202019.pdf
THE HISTORY OF PSYCHIATRIC SERVICES IN SRI LANKA
The indigenous medicine system which existed in Sri Lanka prior to the establishment of modern mental health services during British colonial rule recognized and treated mental disorders. Ayurveda medicine recognized mental disorders as illnesses and had well documented treatment modalities.11 However, there were also native medical practices that attributed causality to astrological factors, sorcery, demon possession and black magic, as well as illness.12 Therefore, certain indigenous treatments became a combination of healing practices, including herbal medicine and astrological and religious ceremonies.13,14
Modern mental health services in Sri Lanka based on Western allopathic medical principles began as asylums under the Lunacy Ordinance of 1873 during the British colonial rule. After establishing two asylums in the city of Colombo, which quickly became overcrowded, a third asylum was completed in 1926 in Angoda, a suburb of Colombo, with 1,728 beds. However, the conditions in the Angoda asylum were criticized by Edward Mapother, professor of psychiatry from the University of London, who was invited by the colonial government to carry out a comprehensive survey. His report, which was published in 1938, proposed 10 recommendations, which laid the foundation for the establishment of a modern mental healthcare system in Ceylon. The Mapother Report recommended the de-centralization of services and the development of a specialist medical service. Following this report, the asylum at Angoda was renamed a mental hospital in 1940 and is now the National Institute of Mental Health, Sri Lanka’s premier tertiary care, specialized hospital for mental health.15
The first outpatient service was established at the National Hospital of Sri Lanka, Colombo, then the General Hospital, Colombo, in 1939.16 Initial mental health services were primarily in and around the Colombo district, located in large institutions. In the mid-1960s, psychiatric facilities were set up in Kandy, Colombo and Jaffna, and over the next 20 years, psychiatrists established more units in major provincial hospitals.
The Ceylon Lunacy Ordinance, originally drafted in 1873, was revised in 1940 and was superseded by the Mental Diseases Ordinance in 1956. A second report of enquiry was published in 1966, which pointed out the weaknesses of the custodial care institutions. The five recommendations made in this report supported the development of a more community-oriented approach, delivered by psychiatrists with the support of psychologists, social workers, mental health nurses and occupational therapists.13 Mental health services gradually expanded over the next few decades and the increased number of positions for psychiatrists was supported by the development of the Department of Psychiatry at the University of Colombo in 1968 and the establishment of the Postgraduate Institute of Medicine in 1980.14,15 However, the substantial number of psychiatrists who left Sri Lanka to work in developed countries after completion of their training presented a challenge in relation to the development of services.13,15
DIRECTORATE OF MENTAL HEALTH
At national level, the Directorate of Mental Health is the central organization of the Ministry of Health, executing the national mental health programme. The directorate is responsible for the development of technical strategies and guidelines, policy development, the development of annual operational plans and budgets, resource mobilization and capacity building in collaboration with the relevant sectors, together with the monitoring and evaluation of the national mental health programme.16
MENTAL HEALTH POLICY (2005 TO 2015)
A mental health policy was drafted by the Sri Lanka College of Psychiatrists and accepted by the government of Sri Lanka in 2005, with the objective of establishing a comprehensive and community-based service to optimize the mental health of the Sri Lankan people.
Seven areas of action were identified that included management at national and provincial levels, the organization of services, human resources development, research and ethics, the National Institute of Mental Health, tackling stigma and promoting mental wellbeing and mental health legislation.
This policy helped to direct the development of mental health services, however, all targets had not been achieved at the end of the defined time period. For example, the recruitment and training of allied mental health professionals continue to lag behind, while the mental health act is still in the process of being reviewed.
The policy recognized the administrative district as the basic service unit and planned for a minimum of one acute psychiatric inpatient unit based in each District General Hospital, as well as a rehabilitation unit for each district. Small divisional hospitals, situated in each MOH area, were to have a primary community mental health centre (PCMHC) comprising a medical officer of mental health (MOMH), community mental health nurses and a community support officer.17
The rapid expansion of services in the psychiatric sector in Sri Lanka is summarised and captured graphically on the website of the Mental Health Directorate of the Ministry of Health in Sri Lanka.18
Two further events in contemporary history affected the provision of mental healthcare in Sri Lanka.
The first was a protracted civil war against the Liberation Tigers of Tamil Eelam (LTTE) over a period of 26 years from July 1983 until May 2009. The armed conflict was mainly in the northern and eastern provinces and severely disrupted health services in the region, but the trauma of war affected the entire country.18
The second event was the Indian Ocean tsunami, which hit the southern and eastern coast of Sri Lanka on 26 December 2004, killing an estimated 35,000 people and displacing more than 515,000 from their homes.19
These two events directly impacted mental health in Sri Lanka by weakening the existing infrastructure for mental healthcare provision in the affected regions and increasing the risk of mental health problems among the population at the time. However, this also led to a renewed focus on community-based care.20
CURRENT PSYCHIATRIC SERVICES IN SRI LANKA
The psychiatric care workforce includes consultant psychiatrists, MOMHs who have either completed a three-month special mental health training or a one-year-diploma in psychiatry, psychiatric social workers (PSWs), trained, designated community psychiatry nurses (CPNs), who are nursing officers with a 6 month training in psychiatry, occupational therapists (OTs) and a variety of other workers including volunteers.
Only three clinical psychologists were available in the state sector in the whole of Sri Lanka in 2012 and they were all attached to universities.21 No ‘clinical psychologist’ post exists in the cadre of the Ministry of Health to date, due to various factors including the dearth of trained clinical psychologists in the country. There have been discussions to recruit psychologists who have master’s degrees in clinical psychology to the health ministry as an interim measure, until trained and qualified clinical psychologists are available.22
All the categories have increased cadre numbers gradually over the years, but significant shortages still remain.23
Table 4 and 5 summarize the current status of psychiatric services in the country (Table 4, Table 5).
Table 4. Health professionals working in the psychiatry sector per 100,000 population
|
Category of Staff |
2005 |
2011 |
2017 |
|
Psychiatrists (Specialists) |
0.2 |
0.29 |
0.52 |
|
Medical officer of Mental Health and Diploma holders (non-specialists) |
* |
0.75 |
1.47 |
|
Nursing Officers |
1.8 |
2.92 |
3.28 |
|
Psychologists |
0.02 |
0.09 |
0.25 |
|
Psychiatric social workers |
0.07 |
0.33 |
0.28 |
|
Occupational therapists |
* |
0.19 |
0.22 |
|
Speech therapists |
* |
* |
0.05 |
|
Community psychiatric nurses |
* |
* |
0.18 |
|
Other paid mental health workers |
* |
* |
1.04 |
* Data not available
Source: Mental Health ATLAS 2017 [Internet]. [cited 2021 Aug 14]. Available from: https://www.who.int/publications/i/item/9789241514019
Table 5. Psychiatry care facilities per 100,000 population
|
Category of Staff |
2011 |
2017 |
|
Psychiatric beds in mental hospitals |
0.10 |
4.97 |
|
Psychiatric beds in general hospitals |
0.20 |
3.96 |
|
Mental health outpatient facilities |
1.36 |
* |
|
Day treatment facilities |
0.12 |
* |
|
Community residential facilities |
0.05 |
1.33 |
* Data not available
Source: Mental Health ATLAS 2017. Accessed August 16, 2021. https://www.who.int/publications/i/item/9789241514019
COMMUNITY-BASED PSYCHIATRIC CARE IN SRI LANKA
The first outpatient clinic in Colombo district was established in 1939, which was followed by other hospital-based clinics in selected major cities. As the focus shifted from hospital-based care to community care, district hospital-based clinics were established in the latter part of the 20th century. Moreover, various elements of community psychiatry such as outreach clinics, residential intermediate rehabilitation centres, home-based care and community resource/ support centres gradually came into existence.24
This gradual evolution contributed to the lack of a clear demarcation between hospital-based psychiatric services and community-based psychiatric services, as both are carried out by hospital-based mental health teams headed by a consultant psychiatrist. This is further complicated by the presence of certain officials and service provision centres that cannot easily be categorized as hospital-based or community-based.25
To an outside observer, the Sri Lankan community-based psychiatric care system can be explained in two ways, according to the content of the service and the organization of care delivery.
Content of community-based psychiatric care
Community mental healthcare is provided for all age groups and for all kinds of mental illnesses, but this treatment mainly caters for adults with severe mental illnesses such as schizophrenia, schizoaffective disorder, bipolar affective disorder, recurrent depressive disorder and substance use disorders.
The types of services included here are outreach clinics, residential rehabilitation facilities, domiciliary care, helplines and community support centres.
Outreach clinics
At present, the main mode of delivery for community care is through outreach clinics held at peripheral, and sometimes, remote, healthcare centres. An example of such a clinic is the Colombo-15 community psychiatric clinic, which opened in 2010.25
In similar clinics functioning in other areas of Sri Lanka, psychiatric inputs are provided by medical officers under the supervision of the district psychiatrist based at the district hospital, who usually visits the clinic at least once a month or more frequently. These clinics mainly function as follow up services for stable patients with long-term mental illnesses and as screening services, which send seriously ill patients to clinics manned by the specialist psychiatrists of the district hospital, located in the main city of that district.
According to the Mental Health Policy of Sri Lanka (2005–2015 and current policy draft version), there should be at least one community psychiatric centre or community psychiatric clinic in each MOH area, which is the smallest health administrative unit in the country.26 There are 342 MOH areas in Sri Lanka, with an average population of around 60,000.
Residential rehabilitation facilities at district level
Intermediate-stay residential rehabilitation facilities have been expanded district-wise over the last two decades in many districts, from one in 2000 to 22 in 2017.27 Most of these centres are hospital-based and are under the supervision of the psychiatrist based at the district hospital. Some of these units such as the Unavatuna District Hospital in Galle (Southern province) and the Kandana District Hospital in Ragama (Western province) cater for patients with significant psychiatric disabilities, due to disorders such as schizophrenia and other psychotic disorders, severe mood disorders, severe personality disorders, mental retardation, acquired brain injuries and other organic brain disorders. In addition to such government-funded rehabilitation centres, non-governmental organizations such as ‘Nest’ and ‘Sahanaya’ also offer residential mental healthcare facilities.28
There are seven state run residential treatment facilities for alcohol use disorders in seven districts.16
Although there are a number of long-term residential treatment facilities for patients with substance use disorders run by the private health sector, the standards of care and effectiveness in these centres are questionable. Some of these facilities follow religious practices in managing substance addiction and withdrawal, rather than evidence-based practices. The few centres run by government agencies such as the National Dangerous Drug Control Board are regulated more effectively and have a higher standard of care.29,30
Home-based or domiciliary care
Home visits for medical, social or functional assessment and for treatment delivery, such as the administration of depot antipsychotic injections are carried out by the hospital-based multidisciplinary teams as necessary.31 However, the level of systematic delivery of such services varies in different parts of the country. Home visits are undertaken by the mental health teams, headed up by a consultant psychiatrist stationed in the district hospital, who will even travel to the remotest regions in the catchment area.
Crisis care services
Sri Lanka does not have a formal crisis care team in its community mental health set-up. In comparison to the West, the very different social set-up in Sri Lanka, where most people live with their families and extended families means that family provides non-specialized, immediate psychological support in times of personal crises. This may be why a mental health crisis team has not been of great need. However, the system of community mental healthcare is such that anyone can walk into their nearest primary care or other hospital and request a mental health assessment. Such persons will be seen by the MOMH or the consultant psychiatrist. Therefore, there is no significant delay in accessing mental healthcare in Sri Lanka.22
Psychological services
The cadre in the mental health services of the Ministry of Health does not currently include psychologists, but this is in the process of being amended. Therefore, there is no formal psychological service available nationally except in a few teaching hospitals, where either a psychologist attached to a university unit or psychiatrists provide such services. All psychiatrists are trained well in common psychological therapies as part of the postgraduate curriculum, and they make use of this competence in their practice. CPNs, PSWs and OTs in larger psychiatric units are trained in cognitive behaviour therapy for anxiety disorders and depression, and work as therapists in addition to the psychiatrists.32
Phone helplines
A national mental health helpline, 1926, was introduced by the National Institute of Mental Health of Sri Lanka in 2018, which is toll free and available to the public 24 hours a day and seven days a week.33 Prior to the establishment of this national helpline, small-scale local helplines, which were established by mental health facilities in the regional hospitals, did improve the link between services and the community in the regional areas of Sri Lanka. An example of such a regional helpline was the mental health triage and support telephone service at Ampara General Hospital, which was established in 2008.34
Community resource/ support centres
Community support centres are drop-in facilities that provide day patient services, information and psychological support/ input.32 However, to date, they have failed to gain crucial support or extensive utilization. It may be possible that other services and community points such as meetings at temples/ kovils/ churches/ mosques may be fulfilling these needs better amidst the dearth of infrastructure and human resources that are needed to run such community support centres in most areas of Sri Lanka.
The National Council for Mental Health, “Sahanaya”, is a well-established community day centre operated by a non-governmental organization, which provides community support for the mental health needs of the public and fills the gaps arising from a limited availability of government funded community resource centres.35
Table 6 summarizes the mental health services available by 2017 (Table 6).
Table 6. Selected statistics of mental health sector in Sri Lanka by 2017
|
Outpatient facilities |
|
|
Mental health outpatient facilities attached to a hospital |
230 |
|
"Community-based / non-hospital" mental health outpatient facility |
20 |
|
Other outpatient facility (e.g. Mental health day care or treatment facility) |
22 |
|
Outpatient facility specifically for children and adolescents (including services for developmental disorders) |
25 |
|
Other outpatient services for children and adolescents (e.g. day care) |
5 |
|
Inpatient facilities |
|
|
Exclusive psychiatry hospitals |
1 |
|
Psychiatric units in general hospitals |
31 |
|
Residential care facilities |
23 |
|
Inpatient facility specifically for children and adolescents |
3 |
Source: Mental Health ATLAS 2017. Accessed August 16, 2021. https://www.who.int/publications/i/item/9789241514019
ORGANIZATION OF COMMUNITY-BASED PSYCHIATRIC CARE
Human resources
Multidisciplinary teams including MOMHs, CPNs and PSWs, led by a consultant psychiatrist, deliver all of the aforementioned community-based care, in addition to hospital-based care. These teams are primarily based at teaching, district and base hospitals, as psychiatrists are only appointed to these hospitals. At least one such team is available in each of the 24 districts in Sri Lanka.36
CPNs who have undergone specialist six-month training in both inpatient and community settings are fulfilling more prominent roles in the delivery of psychiatric care in the community, as they grow in numbers.
As there was a dearth of PSWs, development officers carrying out administrative responsibilities in the health sector were converted to PSWs following a training period of three months. They were appointed to work with the community mental health team in the area in which they were employed.
Use of non-medical/ non-health sector personnel to offer services to the community
One of the challenges in providing mental healthcare in Sri Lanka is the low level of mental health literacy, especially in rural areas, and the reluctance to seek help due to stigma.37 A poor financial status, as seen in rural communities, understandably results in fewer follow up meetings too.
Different mental health services across the country have used various innovative methods to tackle this problem of taking mental health services to people’s doorsteps.
The northern and eastern provinces, which were the hardest hit during the long running terrorist conflict in Sri Lanka enrolled CSOs, who were from the community, in the mental health sector. They were paid an allowance but were not part of the national cadre in the mental health sector.31,34
Certain community psychiatric services temporarily recruited volunteer community support officers (CSOs) from the community during the post-tsunami period, when a large number of service providers were needed.9
Other mental health services utilize volunteers from the community and/ or field-level public officers from the non-health sector to coordinate services and to provide administrative, financial and welfare services support. As these non-health sector individuals (e.g., from the local civil administration) are from the community they serve, they are well accepted and well placed to help people with mental health needs and improve mental health literacy. It is important that the mental health team incorporate these as individual volunteer team members, rather than as a service or an organization providing services.
Some psychiatric services currently utilize these field-level government officers as unpaid volunteer case managers in the community (e.g., in the Ampara district and later replicated in the Hambanthota district).25,34
The sustainability of involving volunteers in the provision of services is questionable but seems to have worked in the case of Sri Lanka.
Sharing of trained mental health professionals within the district
The fewer than optimum number of mental health professionals in relation to the population is dealt with in different ways by different mental health teams. One mental health team comprising CPNs, PSWs, few MOMHs and one or two consultant psychiatrists cover the entire district, by attending the various clinics held at primary care level in the divisional hospitals in their areas, in addition to providing services at inpatient and outpatient hospitals with a larger base and district general hospitals.
This sharing of resources ensures that all areas of the district are served in an equitable manner. This also makes follow ups easier as the same team is involved in inpatient and outpatient care.
The disadvantage is the heavy burden of providing care for an entire district with a limited number of staff, which may lead to an increased burnout rate.
Funding
As the main psychiatry teams who deliver hospital care are also involved in the delivery of community care, there is no clear-cut, separate funding mechanism for community-based care. However, some of the services in the community are funded by provincial health authorities. For example, the transportation of the specialist psychiatrist and team from the main/ district hospital to remote clinics is provided by the provincial health service.
The extent of the provision and support for mental health services depends to a large degree on the budgetary allowance from the provincial government, which will differ from province to province.9
The lack of a separate mental health budget is a major drawback in Sri Lanka. A small percentage of the non-communicable disease (NCD) prevention allocation from the national health budget and other international funding projects are the main sources of funding for mental health activities in the country. This significantly impinges on the systematic expansion of the services and the infrastructure development, including transport services, medical supply maintenance and human resource development.22
Legal backing
The current mental health legislature of Sri Lanka, dating back to the Lunacy Ordinance of 1873 and amended in 1956, has little or no provision for community-based care. This legislature does not provide legal cover for involuntary treatment in regional hospitals or in the community, which significantly hinders an effective treatment framework within the peripheral mental health services in Sri Lanka today.
Link with primary care
In each district, outreach clinics are based in selected divisional hospitals which are primary care units, but these clinics do not exist in all divisional hospitals. Therefore, the link between primary care units and community-based mental services is not uniformly present countrywide. Generally primary healthcare staff will identify and refer individuals for psychiatric assessments.21
Link with other psychiatric care services within the district
There is no division within teams providing community-based and hospital-based services, as it is the district psychiatrist that provides leadership in relation to all aspects of mental health services in a particular health administrative district.36
Non-governmental organizations and professional organizations
Community mental health services liaise with the different non-governmental organizations active in the community they serve, where appropriate.25,35
A number of non-governmental organizations provide different types of supportive services for those with mental health issues. However, most of these organizations are based in the capital, Colombo and in other major cities.23
The Sri Lanka College of Psychiatrists is one of the main professional organizations which liaises closely with the Ministry of Health and the Directorate of Mental Health, to bring about the improvement of mental health services in the country. The College, in addition to its involvement in training mental health professionals of all categories, is involved in reviewing mental health legislature and mental health policy planning, as well as organizing the infrastructure and services throughout the country.38
WAY FORWARD
Mental health policy and legislature
The mental health policy after 2015 is in the process of being reviewed, however, this has not been finalized, which has led to a lag in the improvement of mental health services. A new mental health act is in the process of being enacted to improve and replace the previous Mental Diseases Ordinance of 1873, so that the legislature addresses current and future mental health needs.16
Human resource training, recruitment and retention
Increasing the cadre positions and training allied mental health professionals are ongoing challenges, especially in the face of a restricted health budget. However, this is recognized by the mental health directorate as a need.18 Retaining allied mental health professionals (CPNs, PSWs, OTs, MOMHs) other than psychiatrists in mental health services is difficult, as they come under a general scheme for transfers and promotions in a similar manner to all other professionals in the public health sector. Addressing this effectively is necessary but this would require a change to the government recruiting and transfer rules and policies, which is unlikely to happen imminently.
Administrative backing
The fact that most of the health services in the country are under provincial governance means that local politics and priorities are in operation, which are different from national priorities. This results in differing budgets, impacting the services that are offered in different provinces. While some provinces actively support mental health service provisions and development, others may not. Therefore, there is a discrepancy in the service provision between different parts of the country.
Monitoring and evaluation
A lack of built-in monitoring and the absence of critical evaluation of the effectiveness of services is another drawback in further improving established systems.9 Therefore, key performance indicators (KPIs) and outcome indicators need to be developed for community services. Research and audits are taking place but should be encouraged further. Provincial level and district level reviews of services which occur regularly are not formally evaluated.
Providing encouragement and opportunities for those who implement successful community models and giving others the chance to learn from peers working in different areas of the country where they have been successful are crucially important. Moreover, establishing pathways for the career development of all categories of staff and supporting the health of the workforce to prevent burnout are equally vital, in order to sustain these systems.
DISCUSSION
Historically, when the transition of mental healthcare from asylums and large mental hospitals to services in the community was initiated worldwide in the mid-20th century, this led to many debates and criticisms within the specialty.38,39 Different countries offer different models of community services with varying levels of success or failure. Several models of community mental healthcare have been proposed over time.40-42 However, the overall consensus is that there is no one universal public health model that fits all countries.43
The World Health Organization (WHO), recognizing the treatment gap in mental health services globally, produced guidance for mental health policy and service development in 2009. This pyramid model of care aims to help countries build or transform their mental health services, in a five-stage model to: promote self-care, build informal community care services, integrate mental health services into primary healthcare, build community mental health services, develop mental health services in general hospitals and limit the number of psychiatric hospitals.44
The model of mental health services in Sri Lanka is compatible with the WHO model and the improving statistics bear witness to the way in which this system has been effectively implemented.
However, going beyond this recommended model, the mental health services in different parts of Sri Lanka have managed to further adapt to the needs and availability of resources in the areas they serve, leading to slight but important differences in the organization and delivery of care within the country itself.
CONCLUSION
Sri Lanka has implemented a community mental health system based on the WHO recommended model. The different stakeholders led by the Ministry of Health are working together to improve the quality of the services. Further enhancing this model of care, the mental health professionals providing services in different parts of the country strive to improve their services, by utilizing the resources available in their area, rather than being limited to the resources made available by the government or the system. This has led to unique differences in the way in which services are offered in different areas of the country, which the authors view as a positive feature of the evolving community mental health service model in Sri Lanka.