INTRODUCTION
In Indonesia, the COVID-19 pandemic began in March 2020 and is still ongoing as of April 2022. The government has taken various measures to overcome the its effects, including implementing PSBB (large-scale social restrictions), transitional PSBB, and PPKM (enforcement of restrictions on community activities) (up to four-level). Despite all measures taken, the incidence of COVID-19 remains high in Indonesia.
There are three significant impacts of the COVID-19 pandemic that were felt globally: the economic impact (massive layoffs and reduced salaries), the environmental impact (industrial closures, tourism, etc.), and the psychological impact (increased fear of death, loneliness, and issues related to future security) [1]. Despite causing a severe economic downturn, the environmental effects of the COVID-19 pandemic were rather positive due to reduced levels of pollution across the globe [1, 2]. The psychological impact of the pandemic, in turn, is of particular concern to many researchers, especially in the social and health sciences. Many studies report that the COVID-19 pandemic has had a negative impact on mental health [2–11], triggering anxiety, stress, depression [12–19], loneliness, and worry [20–23]. In addition, a study of 157,213 participants living in America concluded that calm, happiness, and optimism decreased during the COVID-19 pandemic [3].
Studying the state of mental health during the COVID-19 pandemic has become highly relevant and important, especially amongst the elderly population. The elderly population is deemed to be the most vulnerable to the effects of the pandemic [24]. It has been shown that more than 80% of the deaths caused by COVID-19 in America were among people over the age of 65 years (CDC COVID-19 Response Team, 2020). Those who are aged 60 had the highest level of confirmed deaths compared to other age groups. Even in Indonesia, the number of COVID-19 deaths as of 5 November 2021 had reached 143,534, including the elderly population (https://covid19.go.id/peta-sebaran-covid19).
The higher the mortality, the more worried the population seems to be. This is evidenced in research reports indicating high rates of anxiety in the elderly with comorbidities such as hypertension, heart disease, and diabetes mellitus [26]. Other studies report that increased rates of mental health problems were caused by social isolation, impacting their bio-psycho-social vulnerability [27]. In particular, Lumbantoruan et al., 2021 defined that social isolation leads to loneliness, which increases the risk of depression, anxiety disorders, and suicide, especially among elderly patients living in nursing homes. Similar results were reported by Stolz et al., who interviewed 557 participants aged 60 years and over, showing that loneliness increased during the lockdown. Another factor that affects the mental health of the elderly is an attachment to God. Individuals believe that their closeness to God will provide a sense of security and help them in times of difficulty [29]. Homan [30] and Kent et al. [31] demonstrated that there is a link between attachment to God and mental health. Individuals with a secure attachment to God can treat themselves with kindness and care, especially when facing severe problems.
Although there are studies examining the effect of the COVID-19 pandemic on the mental health of the elderly, this research topic has barely been studied in the context of Indonesia. The specific purpose of this research is to examine the mental health status of the elderly during the COVID-19 pandemic in Indonesia during the implementation of the four-level PPKM system and the factors that affect their mental health, such as loneliness and attachment to God.
METHOD
Study design
A sequential explanatory form of mixed-method approach was adopted for this study. Using this approach allowed the combination of quantitative and qualitative elements in a sequential manner and the building of subsequent phases of the research on what had previously been determined. In particular, the researchers first conducted quantitative research, analyzed the results, and then explained them in more detail using qualitative research [32].
Sampling
Incidental sampling was chosen as a sampling strategy for this study. Participants in this study found it difficult to communicate well, so the selection of participants was based on communication skills. Interviews were conducted with the elderly participants who had extreme high and low mental health status, as based on the survey.
Recruitment
We recruited participants by spreading the recruitment link online. We approached colleagues, friends, and psychology students who have elderly family members and asked them to act as guides when completing the questionnaires. Each participant signed a consent form before completing the questionnaire.
Procedure
We used Google Forms to share the above link with colleagues, friends, and psychology students. An online format was chosen to minimize any risk of spreading the COVID-19 virus. After the data was collected, we analyzed the data using mental health level categorization. The data collected was also used to determine potential participants for the planned interviews. Interviews were conducted by psychology students whom we had befriended beforehand.
Measurement
Mental Health Inventory (MHI)
MHI-5 was chosen as a data collection tool to measure the mental health status of the elderly. The MHI-5 is a shortened version of the 38-item based on fundamental theory [34], then expanded to five items [35]. This measurement tool reveals two important aspects: psychological well-being (2 items) and psychological distress (3 items). The MHI-5 has a reliability value of 0.67.
Attachment to God
Attachment to God was measured using the Muslim Spiritual Attachment Scale (M-SAS) developed by Miner et al., which includes 16 items arranged based on four factors: Proximity, Positive model of God, Positive Model of Self, and Separation Protest [36]. Each factor of the M-SAS Scale consists of four items. The M-SAS has a reliability of 0.62.
Loneliness
Loneliness was measured using the University of California, Los Angeles (UCLA) Loneliness Scale 6, also known as ULS-6. The ULS-6 measuring instrument was developed by Hudiyana et al. [37]. The ULS-6 measuring instrument has shown good quality in terms of measuring loneliness in cross-cultural studies and has been tested in three countries, namely Indonesia, Germany, and America. ULS-6 has a reliability of 0.89.
Guide Interview
In-depth interviews were used as a data collection tool. The interview guide was developed following Veit and Ware [34], indicating that mental health is measured based on two opposing dimensions. The positive dimension is represented by psychological well-being and the negative dimension by psychological distress. The interview guide is shown in Table 1.
Table 1. Interview Guide
|
No |
Question |
|
1 |
How did you feel during the COVID-19 pandemic? |
|
2 |
What makes you feel peaceful and calm during the COVID-19 pandemic? |
|
3 |
How can you stay happy during the COVID-19 pandemic? |
|
4 |
What made you feel very sad or uneasy during the COVID-19 pandemic? |
|
5 |
What do you do when you feel sad and uneasy during the COVID-19 pandemic? |
Data analysis
Data from two different approaches was analyzed separately following the guidance offered by Creswell and Creswell [32]. The analysis was completed via three steps. Firstly, quantitative data was analyzed using JAMOVI to categorize it and create correlations between variables and perform regression analyses. Secondly, qualitative data was analyzed via the content analysis. Content analysis includes several steps such as coding of the interview transcript, merging codes into categories, and developing themes [37]. Thirdly, quantitative and qualitative results were integrated.
RESULTS
Participants
Overall, 82 elderly individuals with an age range of 60 to 90 years old were recruited for the purposes of the quantitative part of this study. The majority of participants were women (73.2%). Quantitative sample characteristics are shown in Table 2.
Table 2. Quantitative sample characteristics
|
Demographics |
Levels |
Counts |
% of Total |
Cumulative % |
|
Gender |
Man |
22 |
26.8% |
26.8% |
|
Woman |
60 |
73.2 % |
100.0% |
|
|
Age |
60–65 |
36 |
43.9 % |
43.9 % |
|
66–70 |
12 |
14.6% |
58.5 % |
|
|
71–75 |
12 |
14.6% |
73.2 % |
|
|
76–80 |
15 |
18.3% |
91.5% |
|
|
81–85 |
4 |
4.9% |
96.3% |
|
|
86–90 |
3 |
3.7% |
100.0% |
|
|
Internal Medicine History |
Not |
44 |
53.7% |
53.7% |
|
Yes |
38 |
46.3% |
100.0% |
|
|
Living with Children |
Not |
23 |
28.0% |
28.0% |
|
Yes |
59 |
72.0% |
100.0% |
|
|
Retirement |
Not |
57 |
69.5% |
69.5% |
|
Yes |
25 |
30.5% |
100.0% |
Further, nine elderly participants with very low (three participants) and very high (six participants) mental health status categories were invited to the qualitative interviews. This was done to examine the differences in the groups’ responses and capture diverse perspectives. Qualitative sample characteristics are presented in Table 3.
Table 3. Qualitative sample characteristics
|
Participant |
Age |
Mental Health Status |
|
participant 1 |
61 |
Very low |
|
participant 2 |
77 |
Very low |
|
participant 3 |
73 |
Very low |
|
participant 4 |
62 |
Very high |
|
participant 5 |
61 |
Very high |
|
participant 6 |
73 |
Very high |
|
participant 7 |
67 |
Very high |
|
participant 8 |
65 |
Very high |
|
participant 9 |
63 |
Very high |
Quantitative result
Intercorrelation between variables
According to the results of correlation analysis, the mental health variable has a correlation with loneliness (R=-0.447, with a significance of <.001). This indicates a negative correlation between mental health and loneliness. This means that the higher the loneliness in the elderly, the lower or worse their mental health. On the other hand, the lower the loneliness in the elderly, the higher or better their mental health. The correlation between attachment to God and mental health did not show the expected results as no significant correlation was found. No significant results were found with regard to the relationship between loneliness and attachment to God (Appendix A).
Regression Analysis
Based on the regression analysis, there is a significant effect of loneliness on mental health (R²=0.20; p <0.001). However, the effect is relatively small. The magnitude of the influence of loneliness on mental health is 20%, while other factors influence the remaining 80% (Table 4).
Table 4. Regression analysis results
|
Model |
R |
R² |
Adjusted R² |
Overall Model Test |
|||
|
F |
df1 |
df2 |
P |
||||
|
1 |
0.44 |
0.20 |
0.19 |
20 |
1 |
80 |
<0.001 |
Qualitative result
We deepen the results of quantitative research with qualitative methods. The results of the interviews can be described according to two major themes, namely psychological distress and psychological well-being.
Psychological distress
Based on the results of interviews with nine elderly individuals, it was found that limited activities (not being able to recite the Qur’an together, visiting neighbors, etc.), being anxious and suspicious of others who may have tested positive for COVID-19 and being unable to visit or be visited by children and grandchildren made the elderly unhappy during the COVID-19 pandemic. Religious activities can be one of the ways to avoid and prevent the elderly from experiencing such sadness, which included prayer, reading the Qur’an, and Dzikr. The elderly also mentioned other activities such as going to the fields or doing productive activities at home. Furthermore, using telecommunications equipment to make voice or video calls with family members who are far away and communicating with children and grandchildren at home were mentioned as useful to avoiding psychological distress. Some example quotations are presented below:
“To avoid feeling sad, I pray, read the Qur’an and do more dzikr”
(Female, 73 years)
“When I feel sad, I pray, recite and pray and do dhikr so that my heart feels joy”
(Female, 65 years)
“…by doing activities in the kitchen and around the yard”
(Female, 63 years)
Psychological well-being
Based on the results of interviews conducted with nine elderly people, what makes them happy and how to prevent from being sad could be evaluated. Doing activities such as going to the fields, making coffee, and selling crackers were all mentioned as helping to maintain psychological well-being. Otherwise, avoiding suspicion (some people tend to hide their positive COVID-19 diagnoses to avoid suspicion), staying connected online with family members, playing with grandchildren, and being cared for were specified as making the elderly happy. Some example quotations are presented below:
“Feel peaceful when you go to the rice fields”
(Male, 61 years)
“Can still communicate with other family members even through the internet”
(Male, 62 years)
“…carry out commercial activities such as selling crackers and making ground coffee”
(Female, 63 years)
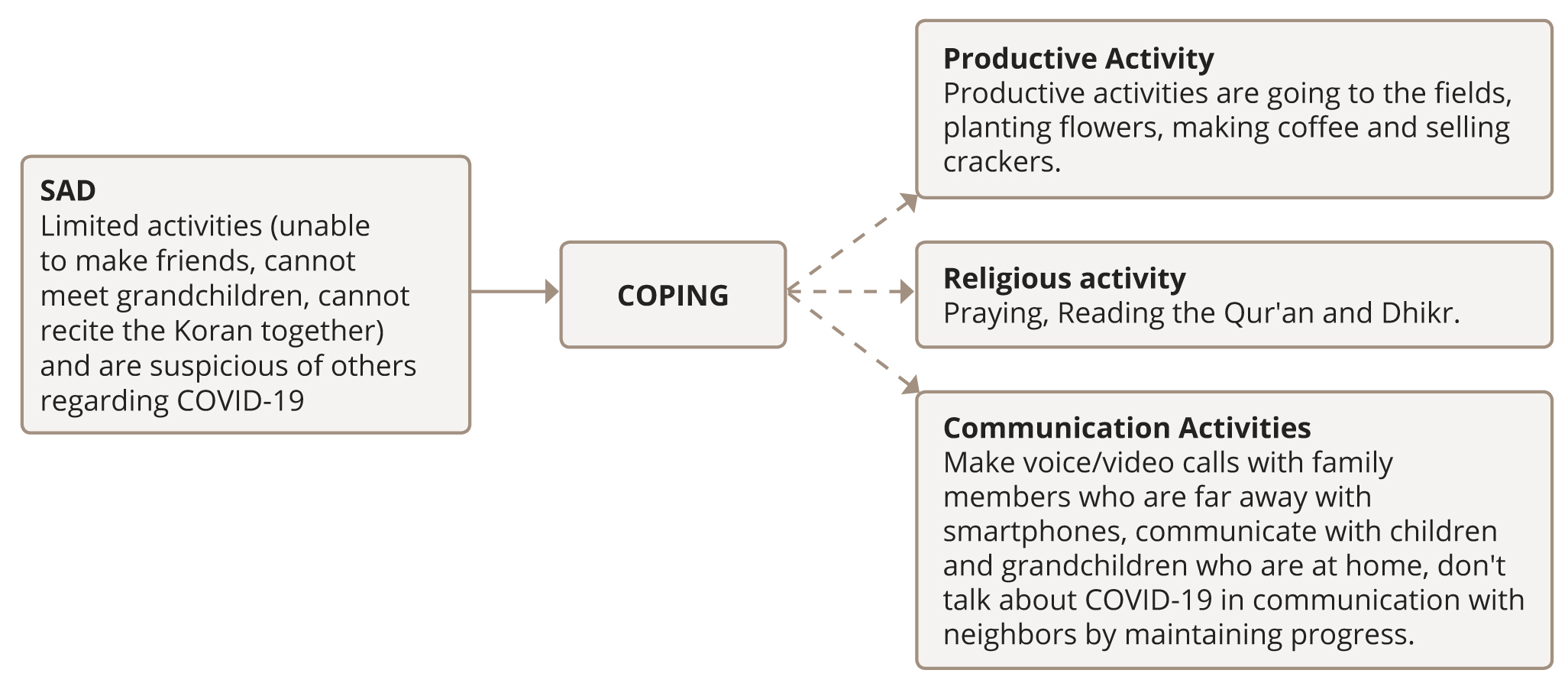
Based on the results of interviews with nine elderly people related to psychological distress and psychological well-being, the flow of themes found in the interviews is shown in Figure 1. It can be seen that elderly individuals could feel sad (part of psychological distress) for various reasons such as limited activities, being unable to meet distant family members, and a suspicion of being among people affected by the COVID-19 virus, then coping with these could be themed into three forms to relieve sadness. The first form of coping includes pursuing productive activities as a form of diversion. The second form of coping is performing religious activities, including prayer, reading the Qur’an, and dhikr. The third form of coping is communication activities, such as making voice or video calls with smartphones, communicating with family members at home, and diverting communication about COVID-19. Coping strategies create happy feelings such as healthy family members, being close to children and grandchildren at home and far away, feeling cared for, and not feeling suspicious in communication with neighbors.
Figure 1. Qualitative research results.
DISCUSSION
Main findings
Based on the results of the quantitative research, mental health is only affected by loneliness. Qualitative results showed that reduced activity, not being able to meet children and grandchildren, and not being able to recite the Qur’an were amongst the main factors triggering sadness among the elderly during the COVID-19 pandemic. Furthermore, we defined that elderly people use productive activities, religious activities, and communication as their main coping strategies.
Strengths and limitations
This study has two main strengths. Firstly, to our knowledge, it is the first study to explore the mental health status among elderly individuals in Indonesia. Secondly, the results of this study can be used as the basis for understanding mental health in the elderly to take further appropriate action.
The results of our study have several limitations. The research sample was defined using non-probability sampling with an accidental sampling technique, so the conclusions drawn are difficult to generalize. The absence of additional training in conducting interviews with the elderly led to difficulties during the interview process, which may have influenced the results.
Comparison with the existing literature
The results of this study generally confirm that psychological distancing causes problems such as feeling lonely [38], especially amongst adults who cannot use technology [39]. Similar results were found among elderly people in Europe who reported a higher loneliness due to physical distancing during the pandemic [40]. Although other studies confirm that loneliness in the elderly occurs only in those with multiple physical and mental health diagnoses, it is associated with reduced loneliness in those with larger social networks [41].
No correlation between attachment to God and mental health was confirmed in this study. In contrast, another study noted that there was an effect of attachment to God on mental health [30, 31]. According to the qualitative data results, in order to cope with loneliness, elderly individuals use worship-related practices, showing their attachment to God. Therefore, we suspect that attachment to God might well be a moderating variable, while religious coping is a mediator between loneliness and mental health.
Implications for future research
We suggest the following implications for future research. Firstly, the attachment to God variable may need to be reviewed using different approaches. Such studies might confirm why Attachment to God has no relationship with mental health status (or indeed otherwise). Secondly, the religiosity variable can be studied further and compared with the attachment to God variable. Finally, considering that Indonesia is known to be a religious country, exploring certain religious concepts could be helpful to a description of how religious concepts influence mental health.
CONCLUSION
This study confirms that the loneliness caused by lockdown is a factor in mental health issues among the elderly population, whereas attachment to God has no apparent effect. The results show that reduced activity, inability to meet children and grandchildren, and inability to recite the Qur’an are the main factors triggering sadness among the elderly during the COVID-19 pandemic. Furthermore, we defined that elderly people use productive and religious activities and communication as their main coping strategies. The implications of this research can be used as a basis or reference for maintaining the mental health of the elderly during the pandemic. The results of the study should be interpreted in light of its limitations with regard to the number of participants and other variables that may have an impact on mental health.