Introduction
A review by the World Health Organization (WHO) noted that the number of unmet mental health needs in the general population is on the increase and that there is a need for a strategy aimed at promoting mental health and pre-empting mental disorders [1]. The WHO also reports that half of mental health problems emerge before the age of 14 [2], whereas the proportion of children with mental health issues ranges from 10 to 29% of their general population [3–5]. Therefore, evaluating the risk of children developing mental, behavioral, and developmental disorders (MBDDs), including autism spectrum disorders (ASDs), as well as detecting such disorders early, has become one of the most important tasks facing public mental health officials throughout the world [6–8].
Screening procedures are recognized as the most cost-effective population-wide preventive strategies for reducing the societal burden of mental illnesses [9, 10]. Although the number of studies focusing on epidemiological screening for mental health issues among children has risen in the last decades [11, 12], the early detection and epidemiology of MBDDs in young children remain insufficiently investigated [13, 14]. Many prospective, longitudinal studies indicate that risk factors and predictors of mental disorders can be identified in the early years of a child’s life [13, 15–18]. Timely identification and treatment of MBDDs is critical for children wellbeing [19] and crucial in preventing the emergence of psychological and developmental problems in later life [20–23]. Hence, screening for MBDDs can contribute substantially to the development of a national medical system of MBDDs prevention, early diagnosis, and timely intervention.
Children mental health is now recognized as an important country-level issue in Russia [24, 25]. According to national statistics, MBDDs, including ASDs, dominate among childhood disabilities [26]. As in other countries, in Russia MBDDs are diagnosed according to the International Classification of Diseases, Tenth Revision (ICD-10). Having acknowledged the importance of preempting the development of MBDDs, including ASDs, in early childhood [27], the Russian Ministry of Health has launched a campaign targeting parents. Under this campaign, parents are entitled to free consultations with child psychiatrists during the first years of their children’s life [24]. This campaign should help parents with preventive advice and assistance in the early detection of metal health issues in their children. Notwithstanding, Russia still experiences a lack of capacity as concerns epidemiological estimations of MBDDs prevalence in early childhood.
Against this backdrop, this study aims to determine the risk of developing MBDDs among young children (18–48 months old) and the prevalence of such disorders in Russia.
Methods
Context
The present study was performed as part of the Russian national epidemiological screening campaign for MBDDs. In Russia, epidemiological screening for MBDDs was initiated by the Ministry of Health and was carried out in two stages, between 2015 and 2019. Firstly, screening of children 16 to 24 months old was implemented in order to assess the risk of developing ASDs in the three largest Russian regions [28, 29]. Secondly, the scope of the screening was extended, with the aim to explore the risk of developing MBDDs of different origins (including ASDs) among children between 18 and 48 months of age across nine regions of Russia (Volgograd, Kirov, Moscow, Novosibirsk, Orenburg, Tver, Chelyabinsk, Yaroslavl, and Stavropol). These nine regions were representative in terms of mean population size and density. Furthermore, these regions were selected for the pilot study because of the presence in them of a well-established pediatric infrastructure, with a sufficient number of capable child psychiatrists. The screening was executed as part of the mandatory clinical examination of children in primary public healthcare institutions. It aimed to cover a maximum number of children, including those with genetic diseases, hearing and other disabilities, who might be at higher risk and in need of a psychiatrist or clinical psychologist for preventive purposes.
Procedure
The two-tiered epidemiological screening approach was developed and adopted for the purposes of the current study. At the first level, the parents of all the children between 18 and 48 months old were questioned using the Russian nationally validated Screening Checklist for Parents for Identification of the Risk of Mental, Behavioral, and Developmental Disorders in Early Childhood (SCPIR) in the abovementioned nine regions of Russia [25, 27]. The SCPIR is similar to the questionnaire developed by Prof. C. Gillberg in the context of Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations (ESSENCE), which aims to cover all types of early developmental disorders [30]. The assessment was carried out in primary healthcare institutions mainly by pediatricians, with the involvement of neurologists, clinical (medical) psychologists, and medical students. We note that a defined risk of MBDDs was not interpreted as a diagnostic category and that it cannot substitute a clinical diagnosis by a psychiatrist.
At the second level, the at-risk children detected at the first level of screening were assessed by a child psychiatrist on a voluntary basis and diagnosed according to the ICD-10 criteria. The ICD-10 criteria were used as special diagnostic classifications. Other classifications, such as the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0-3 or DC:0-5) [31], are not used in Russia. Children diagnosed with MBDDs were kept under the dynamic supervision of a psychiatrist. Children who had not been diagnosed with MBDDs remained under the supervision of a pediatrician, and consultations with a clinical psychologist were recommended in their case in order to forestall any possible difficulty in their cognitive development.
Data analysis
A descriptive-analytical method was used for the purposes of the current study.
Results
In total 595,691 parents (one parent per child) of children aged 18–48 months (born within 2017–2019) were surveyed in nine regions of Russia (Volgograd, Kirov, Moscow, Novosibirsk, Orenburg, Tver, Chelyabinsk, Yaroslavl, and Stavropol regions). The participants were not divided into subgroups based on either theirs or their children’s age. Although the parents had the right to decline to participate in the survey, no refusals were registered. The average screening coverage of the child population of the specified age was 53%, the maximum coverage was in the Orenburg region (80%), in the Chelyabinsk region (68.5%), and in the Volgograd region (66%), and the minimum coverage was in the Novosibirsk region (20%). Low coverage might have been caused by a lack of awareness about the project in some regions.
The analysis of the obtained data has demonstrated that, on average, the risk of developing MBDDs among the child population aged 18–48 months stands at 13.07% (1,307 cases per 10,000). The MBDDs risk indices were found to vary significantly across the regions. The minimum values were noted in Orenburg, Stavropol, and Chelyabinsk regions (3.69%, 4.85%, and 6.7%, respectively), whereas maximum values were registered in the Volgograd, Kirov, and Moscow regions (19.15%, 19.22%, and 23.28%, respectively). Such discrepancies might have to do with the existing issue of uneven access to healthcare services among urban and rural child populations. However, there was no accessible data on the urban and rural child populations that participated in the study, making it difficult to draw conclusions that could stand under scrutiny.
The prevalence of confirmed MBDDs was found to stand at 1.51%, or 151 cases per 10,000 child population aged 18–48 months [32, 33]. Minimum values of this index were observed in the Orenburg (0.51%), Stavropol (0.31%), and Chelyabinsk (0.25%) regions, where the risk of developing MBDDs was also the lowest. The highest prevalence of MBDDs was noted in Kirov (3.57%) and Tver (5.24%) regions. Although the age coverage was similar in all regions, the regions participating in the study differed in their population size and in their level of development of preventive psychiatric and psychological care systems for young children. Kirov and Tver regions are both characterized by relatively small territories and populations, as well as better developed child psychiatric infrastructures. In particular, a specialized system of comprehensive care for children (from 1-year-old) was introduced in these regions in 2010. Considering that an extended diagnosis of MBDDs is based on the work of a multi-disciplinary team of clinical specialists, early introduction of the specialized care system might explain the highest rate of MBDDs found in these regions. The present study’s findings suggest that ASDs prevalence is 0.18%, or 18 cases per 10,000 children population of between 18–48 months of age.
The group of “specific disorders of psychological development” (F80–F83) constituted 60.41% of the sample and prevailed over other MBDDs (Figure 1a). This group included the specific disorders of speech and language development, progress in educational skills, development of motor function, and mixed disorders of mental development. It is important to note that children diagnosed with F80–F83 are of special interest to clinical psychologists, psychiatrists, and pediatricians because of the possible deterioration of their state in the absence of adequate help and treatment. The next two most frequently observed groups were behavioral disorders, including hyperkinetic, emotional, and behavioral disorders (F90–F98), comprising 17.08% of the overall sample, and the pervasive developmental, general psychological development, and ASDs (F84.0–F84.8), comprising 16.92% of the overall sample (Figure 1a). These groups were followed by mental retardation (F70–F79), comprising 5.54% of the sample. Early-onset childhood type schizophrenia (F20.8xx3) comprised only 0.06% of the sample (Figure 1a).
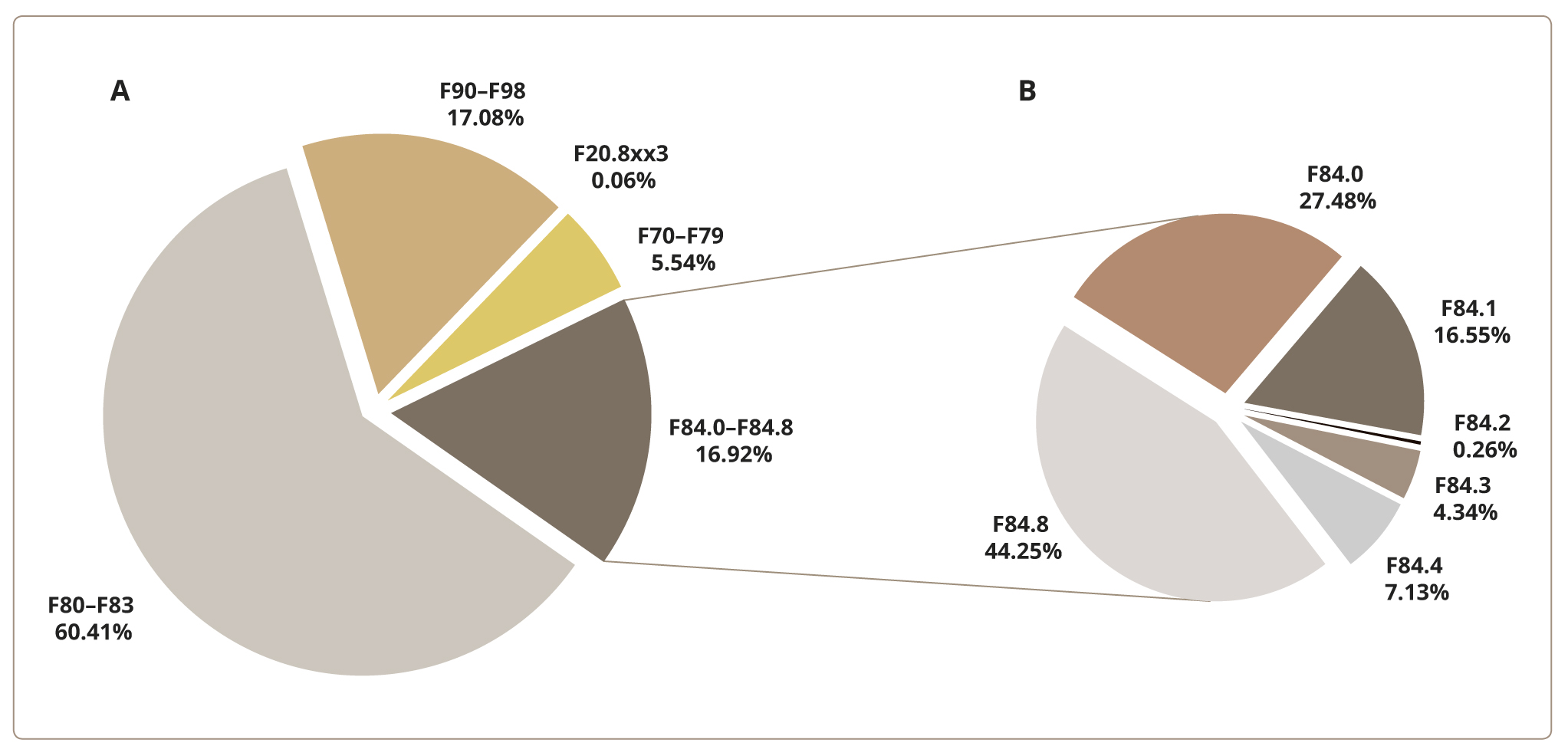
Figure 1. The structure of mental and behavioral developmental disorders, according to the ICD-10, among children 18–48 months of age in nine Russian regions.
A separate analysis of the group of pervasive developmental, general psychological development, and ASDs has shown the following distribution (Figure 1 b): “Childhood autism” (F84.0) comprised 27.48% of the cases; “Atypical autism” (F84.1) — 16.55%; “Hyperactive disorder associated with mental retardation and stereotyped movements” (F84.4) — 7.13%; “Other childhood disintegrative disorder” (F84.3) — 4.34%; and “Rett syndrome” (F84.2) — 0.26%. The prevailing group of “Other pervasive developmental disorders” (F84.8), which comprised 44.25% of the cases, represents a temporary diagnostic category. Only dynamic observation of the children enables further diagnostic specification.
The present study’s findings also suggest that the prevalence of ASDs is 0.18%, or 18 cases per 10,000 of children population between 18–48 months old. In our previous pilot study conducted between 2015 and 2016, the prevalence of ASDs was estimated at 0.05%, or 5 cases per 10,000 child population between 16 and 24 months old (diagnosed according to the ICD-10 criteria) [28]. Thus, estimation of the prevalence of ASDs has increased with the expansion of the age range. This can be explained by the deterioration of the mental state of undiagnosed children without medical help and the appearance of comorbid symptoms.
Discussion
Main result
The present study reveals that the risk of developing MBDDs among a Russian child population aged 18– 48 months stands at 13.07% (1,307 cases per 10,000), whereas the prevalence of confirmed MBDDs among a Russian child population aged 18–48 months is 1.51% (151 cases per 10,000).
Strengths and limitations of the study
To our knowledge, this was the first study assessing the risk of developing MBDDs and the prevalence of MBDDs among young children (18–48 months old) in Russia.
Screening for mental health in children is generally laden with ethical, social, and cultural quandaries [34]. The most screening tools have been developed in English in the United States or United Kingdom; thus, translated versions are needed for use in culturally and linguistically different populations. For example, the translation methods proved to affect selected psychometric properties differing in the various translation versions of the M-CHAT-R [35]. A more accurate cultural adaptation approach may be necessary to maintain relevance with the original instrument. Besides, M-CHAT is designed specifically for ASD, but our study was targeted at a broad MBDD spectrum, and even more so, at revealing the risk group for MBDD development.
The proposed Russian national SCPIR screening checklist enables determination of the risk of developing MBDDs (including ASDs) based on the scientific and practical experience of Russian child psychiatrists and psychologists. This checklist does not require any special training, and the questions on the list are formulated in terms accessible to parents. The Ministry of Health of the Russian Federation has reacted positively to the results of this epidemiological study and has issued Order of the Ministry of Health of the Russian Federation № 396n, which has instructed integration of the screening procedures into the Russian primary care system (since the end of 2019) [36]. However, the association between gender and the risk of developing MBDDs and the prevalence of MBDDs among the children included in the study was not taken into consideration. Therefore, this can be considered as a limitation of the study.
Comparison with the existing literature
The data obtained in our study are comparable with those of a Danish cohort study (diagnoses in which were also made according to the ICD-10 criteria). The Danish researchers reported that 16,164 children (1.76% of a population of 918,280 children in their first four years of life) were diagnosed with mental (0.90%) and/or general developmental disorders (1.05%). The incidence of mental and developmental disorders diagnosed within the first four years of life increased in the following years (1997–2010) and showed complex comorbidities [12].
In a Norwegian population study (n=1555), the highest prevalence of suspected developmental delays was identified in the gross motor area among children 4–12 months of age and accounted for 2.3–8.7% (0.4–4.6% in the fine motor area), whereas the overall prevalence rates of suspected developmental delays varied from 5.7% to 12.3% [14].
A recent meta-analysis has estimated the prevalence of mental disorders among children worldwide [37]. It included ten studies, summarizing data on 18,282 children of 12–83 months of age from eight countries. The pooled prevalence of mental disorders was estimated at 20.1%. The most common disorders were defiant disorder (4.9%) and attention-deficit hyperactivity disorder (4.3%). The study revealed that the epidemiology of mental disorders in children younger than seven years remains a neglected area of research, and that a significant number of young children suffering from mental disorders are in need of appropriate age-adapted treatment [37]. Another review estimated that the prevalence of mental health disorders amongst children aged from one to five years is about 16–18% [38].
When comparing Russian epidemiological data on the prevalence of ASDs with other populations, we noted that information about ASDs prevalence worldwide is mostly available for children above 36 months (older than 3 years old). This might have to do with issues in the development of mental health services for young children and the interest accorded the problems of school-age children and adolescents. Available epidemiological data from Belarus suggests that the prevalence of ASDs is estimated at 5.07 cases per 10,000 children and adolescents in a population aged from three to 17 years [39]. These numbers are similar to the findings in our study but lower than the results obtained in the studies originated in other countries.
Since 2000, the United States Centers for Disease Control and Prevention (CDC) has been actively monitoring the prevalence of ASDs among children aged eight years in eleven states (Autism and Developmental Disabilities Monitoring Network, ADDM). According to the data for 2016, the prevalence of ASDs was 185 cases per 10,000 children aged eight years, of which 33% had severe mental retardation, 24% had borderline mental retardation, and 42% had a medium or high IQ. An increase in the identification of cases with ASDs by 175% was shown compared to the first data obtained in 2000 and 2002 [40]. According to the latest report released by the CDC in 2020, the prevalence of ASDs was 156 cases per 10,000 in a four-year-old children population [41]. Overall, 53% of these cases had mental retardation. It is important to note that the prevalence of ASDs varied widely depending on the US state. The minimum number of 88 cases per 10,000 four-year-old children population was registered in Missouri, whereas the maximum number of 253 cases per 10,000 four-year-old children population was recorded in New Jersey [41]. According to the CDC, the prevalence of ASDs reached 250 cases per 10,000 children population aged three to 17 years in 2016 [42]. However, another US National Health Interview Survey (NHIS) reports an even higher prevalence of ASDs of 276 per 10,000 children population aged from three to 17 in the same year [43].
A recent meta-analysis estimated the pooled prevalence of ASDs in China at 39.23 cases per 10,000 children population (the age of the included subjects ranged from 1.6 to 8 years, with the median age of 4 years). Specifically, the prevalence of autism was estimated at 10.18 cases per 10,000 children population [44], which is close to our estimations in the Russian population. A great gender-related difference in the prevalence was revealed in the Chinese analysis (20.50 cases in boys versus 6.12 cases in girls per 10,000 population) [44]. This interesting observation could be tested in Russian and other populations in the future, because the average epidemiological estimations of ASD in Chinese and Russian child populations are similar.
According to the eleven meta-analyses reflecting the prevalence of autism conducted in 1966–2019, the border between people diagnosed with autism and the rest of the population has been shrinking in the last decade, which affects the increase in figures reflecting the prevalence of ASDs [45]. There is evidence that the broadening of the ASDs concept in terms of the expansion of diagnostic criteria, development of medical services, and awareness improvement plays a major role in explaining the increase in the prevalence of ASDs, although we cannot rule out that other factors might also contribute to the trend [11, 46]. It is worth noting that epidemiological assessments around the world can be influenced by differences in diagnostic approaches, clinical practices, the traditions of medical communities, data sources for statistics, and the availability of medical and rehabilitation care for children. Also, it is important to take into account the influence of ethnic, linguistic, and other characteristics of the population.
It is useful to note that ADDM Network estimates are based on data from various sources (general health clinics, reports from specialized programs serving children with developmental disabilities, as well as from public schools). Further, these data are processed by experienced doctors in accordance with the diagnostic criteria for autistic disorder, Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS), including Atypical Autism and Asperger Syndrome according to DSM-IV-TR (2000). Also, the prevalence of ASD in the US is determined by interviewing families by phone, and currently, by e-mail, based on the subjective assessment of parents and alignment with the DSM criteria (National Survey of Children’s Health, NSCH). Criticisms regarding the estimations of ASD prevalence made by CDC ADDM have been expressed by the research group headed by Professor T.S. Brugha, the UK psychiatrist epidemiologist, who noted that passive sampling analysis is unreliable [47].
According to an Italian child psychiatrist, Professor M. Zappella, the striking differences in epidemiological estimates are associated with the methods used in the examination and assessing of children. The primary method for assessing autism, he notes, should be a clinical examination of the child and family, with possible involvement of psychometric research data [28].
An increase in the number of newly revealed cases with ASD among the world might be due to the changes in diagnostic approaches and emergence of new nosological classifications over the past two decades [49, 29].
Implications for future research and practice
Raising awareness of MBDDs among Russian parents is one of the possible strategies in efforts to move the needle on the issue. Considering that screening procedures are already integrated into the Russian primary care system, children with a higher risk of developing MBDDs need preventive care because of their vulnerability. Creating the required conditions, such as regular consultations with psychologist and other pediatric medical specialists, is essential for a full development of these children.
Conclusion
Screening for the risk of developing MBDDs, including ASDs, in Russia among very young children in the general pediatric population is a promising area of preventive medicine. This initiative allows to develop optimal algorithms for specialized care measures, preventing the development and aggravation of mental health issues affecting children.