Introduction
According to WHO, the average prevalence of autism spectrum disorders (ASD) in children stands at approximately 1 in 100 [1]. At the same time, a significant number of studies conducted mainly in countries with a high standard of living reveal a higher prevalence of autism.
Meanwhile, there is a need for more reliable estimates of the prevalence of ASD that take into account the severity of the affliction, to plan steps in the area of public health and education, anticipating the number of disabilities and the needs in terms of social support programs, as well as setting priorities in the field of research [2].
The term “autism spectrum disorders” per se is not included in the ICD-10, but it is present in the ICD-11, the transition to which is currently underway and is expected to be completed in the next 3 years (by 2025). The catchall concept of “autism spectrum disorder” pools all forms of “autism” cited in the ICD-10: childhood autism, atypical autism, Rett syndrome, other childhood disintegrative disorders (F84.0–F84.3), and Asperger’s syndrome (F84.5). In addition, in the ICD-11, it will become necessary to determine the level of concurrent disorder in intellectual development and the impairment of functional language as part of the core diagnosis for this group of disorders.
The first studies conducted in the 1960s and 70s in Europe and the United States estimated that the prevalence of autism ranged from 2 to 4 cases per 10,000 children [3, 4], which gave the impression that autism was a relatively rare developmental disorder [5].
After the expansion of diagnostic criteria for autism in the 1980s and 1990s, studies of its prevalence predictably showed a significant increase in the number of cases in the population [6–8]. At the beginning of the 21st century, estimates of the prevalence of autism in the United States already stood in the range of 6 to 7 per 1,000 children, which represents a more than 30 times increase compared to 30 years ago [9].
The increase in the prevalence of autism in recent years mainly has to do with the expansion of diagnostic criteria for the disorder and the acceptance of the concept of autism as a spectrum of certain disorders of varying severity [10–12].
Other factors that have been hypothesized to contribute to the increasing number of patients diagnosed with autism include screening and the improved quality of health care in general, as well as an increase in the proportion of children born to aged parents, an increase in the proportion of surviving children with extremely low birth weight, and assortative mating for autism spectrum disorders [7, 13–16].
In addition, it has been recognized that the increase in the number of reported cases of autism has contributed to the expansion of diagnosis among adults, female patients, and high-functioning individuals of both sexes [17].
The latest systematic review concludes that the increase in the measured prevalence of autism in most of the developed world reflects the combined impact of various factors, including increasing awareness on the part of the parent community and the public health response capacity [2].
The upward trend in the diagnosis rates of autistic disorders is also observed in Russia. The total number of people with ASD, according to monitoring in 2018, was 22,953 persons, a 43% increase (6,955 people) in the number compared to 2017 (15,998 people) [18].
It is important to note that, according to various studies, ASD prevalence rates vary widely not only between different countries but also between different regions within countries. Thus, a study conducted in 2018 in the United States by the Autism and Mental Developmental Disabilities Monitoring Network showed that the prevalence of ASD per 1,000 children aged 8 years varied from 16.5 in Missouri to 38.9 in California [19]. A study published around the same time in JAMA Pediatrics showed that children in Florida were diagnosed with ASD three times more often than in Texas — 4.88% and 1.54%, respectively [20]. At the same time, researchers conclude that the actual prevalence of autism does not significantly depend on geographic, racial, or socioeconomic factors.
However, these factors may affect the detection of the disorder. Research results show that the number of established diagnoses correlates with the level of awareness of the main manifestations of ASD among the general public and professional community, in particular. The timeliness of the diagnosis and the quality of care depend on the number of trained specialists, the availability of formalized screening procedures, and the modern medical and educational services available in the region for families raising children with ASD. Living near urban centers with access to quality medical care and special education programs has a beneficial effect on the quality of life of patients with ASD: therefore, there is a need to attract additional resources in the development of monitoring programs and assistance to families from vulnerable low-income groups [19].
Thus, a comparison of autism prevalence rates in a country helps identify regions with limited access to diagnostic services and adequate medical care. It also stands as a way to highlight the need to improve the overall professional level, to zero in on shortcomings in the organization of screening activities and public awareness, and substandard special educational conditions, and it points to a likelihood of the presence of socioeconomic barriers for families on the path to diagnosis. Our study aimed to estimate the number of individuals meeting the diagnosis criteria of ASD in Russia. In addition, we specifically investigated the differences in the number of registered individuals with an established diagnosis in the constituent territories of the Russian Federation.
Methods
A retrospective observational study was conducted to assess the number of individuals with established diagnoses corresponding to ASD in the Russian Federation and its constituent territories, and the 2020–2021 data of form 12 “Information on the Number of Diseases Registered in Patients Residing in the Service Area of a Healthcare Institution” (report form to Federal State Statistics Service; hereinafter — Form 12) were used. The study did not aim to determine the true prevalence of autism. It was important for us to determine how many patients with an established diagnosis had access to the services needed to resolve their medical, social, and educational issues (disability registration, referral to a psychological, medical, or pedagogical commission, etc.). Therefore, the analysis includes the item of form 12 “The patient is under follow-up at a healthcare facility at the end of the reporting year.”
Form 12, approved in 2019 (Order of Rosstat No. 679 dated November 22, 2019), contains the classes and individual diseases following ICD-10, where the following disorders are combined in line 6.2: childhood autism, atypical autism, Rett syndrome, other childhood disintegrative disorders (F84.0–F84.3. The genetic syndrome is coded under the appropriate rubric (LD90 “Conditions with disorders of intellectual development as a relevant clinical feature”), and a diagnosis of ASD is made by a psychiatrist.
The statistical analysis was carried out in R version 4.1.1 (package tableon). The quantitative parameters were tested for uniform distribution using the Kolmogorov–Smirnov test. Since the distribution was abnormal, we calculated the median and interquartile ranges (IQR) for the quantitative parameters. Comparison of the quantitative characteristics of independent groups was performed using the Mann-Whitney test (when comparing 2 groups) or the Kruskal-Wallis test (≥3 groups). An adjustment for multiple comparisons (q) was calculated to account for multiple hypothesis testing, and the q results should be used to detect significant differences when more than 2 groups are compared. The hypothesis testing was two-sided: p <0.05 values were considered statistically significant.
Results
According to the Department of Monitoring, Analysis and Strategic Health Development of the Federal State Budgetary Institution “Central Research Institute for the Organization and Informatization of Healthcare”, in 2021, 41,307 individuals were under follow-up regime (FU) at healthcare institutions with diagnoses consistent with ASD, which exceeds the figures for 2020 by 5,897 individuals (Table 1). The median number of individuals with ASD under follow-up at healthcare institutions in the constituent territories of the Russian Federation was 21 (14.36) per 100,000 population (Table 2).
Table 1. Number of individuals with ASD under follow-up at healthcare institutions (per 100,000 of the corresponding population)
|
Territory |
2000 |
2021 |
Growth rate, % |
|
Russian Federation |
24.2 |
28.3 |
17 |
|
Central Federal District |
34.7 |
35.7 |
3 |
|
Northwestern Federal District |
11.3 |
13.4 |
19 |
|
Southern Federal District |
22.4 |
32.8 |
46 |
|
North Caucasian Federal District |
14.7 |
19.0 |
29 |
|
Volga Federal District |
19.9 |
23.8 |
25 |
|
Ural Federal District |
28.2 |
32.7 |
16 |
|
Siberian Federal District |
23.6 |
29.6 |
25 |
|
Far Eastern Federal District |
22.0 |
26.1 |
19 |
Table 2. Median number of individuals with ASD under follow-up at healthcare institutions in the Russian Federation (2021)
|
Under follow-up with ASD at the end of 2021 (per 100,000 population) |
Number of Russian Federation regions N=85 |
|
Median (IQR) |
21 (14; 36) |
|
Min-Max |
1.7–178 |
In 2020, the studied indicator exceeded the average Russian level only in two federal districts; the Central Federal District (CFD) and the Ural Federal District (UFD), while in 2021 four such districts had appeared: the Central Federal District (CFD), Southern Federal District (SF), Ural Federal District (UFD), and Siberian Federal District (SFD). There was a significantly lower number of patients with ASD under FU in the North-Western Federal District (NWFD) than the average all-Russia level (by 2.1 times). Low figures, in comparison with the all-Russia level, were registered in the North Caucasian Federal District (NCFD) and Volga Federal District (VFD). In the Far Eastern Federal District (FEFD), the figure is slightly below the Russian average.
There is a pronounced uniformity in the growth rate of the number of individuals with ASD under FU in the federal districts: from an insignificant 3% in the Central Federal District to a high 46% in the Southern Federal District (Table 1).
A steady upward trend in the number of individuals with autism has persisted since 2014 both in the Russian Federation, as a whole, and in the federal districts. However, the indicator still differs significantly (the all-Russia one by almost 40 times) from the global median prevalence of ASD.
Table 3 shows the percentile distribution of the number of individuals with ASD under FU in the constituent territories of the Russian Federation, indicating its extremely heterogeneous nature. In the interquartile range (25; 75th percentile), there are 38 regions with 15 to 36 individuals with ASD under FU per 100,000. The all-Russian indicator is also in the same range. The distribution below the 25th percentile includes 26 constituent territories of the Russian Federation — this is slightly less than a third (31.8%) of all districts — with the number of individuals with ASD under FU ranging from 1.7 to 14 per 100,000 population.
Table 3. Distribution of the number of individuals with ASD under FU in the territories of the Russian Federation by percentiles
|
Indicator |
Regions with prevalence >75th percentile N=21 |
Regions with prevalence <25th percentile N=27 |
Regions with prevalence within 25-75th percentile N=37 |
p-value1 |
q-value2 |
|
2021 (absolute number) N |
21 |
26 |
38 |
<0.001 |
<0.001 |
|
Median (IQR) |
604 (315; 1129) |
113 (68; 184) |
264 (176; 455) |
||
|
Min-Max |
25–5367 |
6–691 |
78–1352 |
||
|
2021 (per 100,000 population) N |
21 |
26 |
38 |
<0.001 |
<0.001 |
|
Median (IQR) |
51 (42; 57) |
12 (8; 13) |
24 (19; 27) |
||
|
Min-Max |
37–178 |
1.7–14 |
15–36 |
Note: 1 Kruskal-Wallis rank sum test, 2 False discovery rate correction for multiple testing.
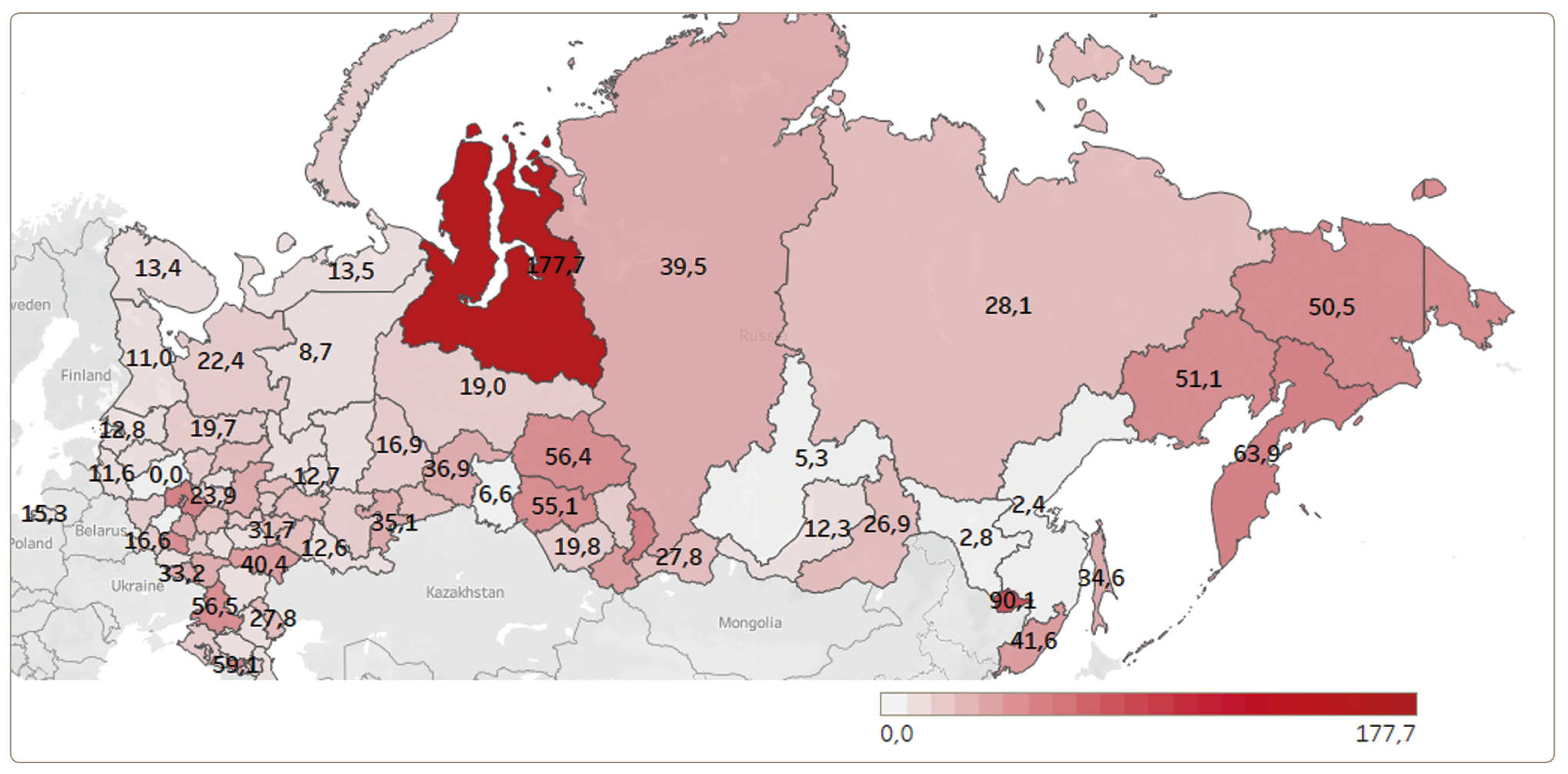
The minimum number of individuals with autism under FU (per 100,000 population) was registered in the Kaluga Region, Khabarovsk Territory, Amur, Irkutsk, and Omsk Regions (Figure 1).
Individuals with ASD under FU above the 75th percentile were registered in 21 regions of Russia. The maximum number of individuals with ASD under FU (per 100,000 population) was registered in the Kabardino-Balkarian Republic, the Republic of Khakassia, the Kamchatka Territory, the Jewish Autonomous Region, and the Yamalo-Nenets Autonomous Okrug.
There are significant regional differences (104.5 times) in the studied indicator: from the minimum in the Kaluga region (1.7 per 100,000) to the maximum in the Yamalo-Nenets Autonomous Okrug (177.7 per 100,000).
Discussion
The upward trend in the number of patients diagnosed with ASD persists both in the Russian Federation, as a whole, and in each federal district, which reflects the widespread improvement in the quality of diagnostics. At the same time, the growth rates in the proportion of individuals with ASD in different Russian territories differ significantly (104.5-fold differences in the ASD prevalence). In other words, the likelihood of being diagnosed with ASD depends on one’s place of residence. Delayed (late) diagnosis of autism or interpretation of the condition as other diagnostic rubrics (mental retardation or schizophrenia) severely limits the ability of patients to access educational services and certain therapeutic interventions. In Russia, decisions in the education system are still made based on the medical model (the educational program depends on the diagnosis), which means that when developing an adapted educational program (AEP), the child stands the risk of being deprived of a range of services that he/she could have otherwise received had he/she been diagnosed with autism.
Although our study provides comprehensive information on the mapping of the service usage in ASD across the Russian Federation, it has several limitations. For objective reasons (specific to official state statistics), our study did not include patients who were diagnosed with Asperger’s syndrome (F84.5), which undoubtedly affected the total number of patients, but to a lesser extent affected the comparative analysis of the substantive problems encountered in the territories of the Russian Federation. At the same time, the Rett syndrome is included in ASD, because the discovery of its genetic cause does not negate its typical clinical manifestations, which determine the need for medical, educational, and social services.
We suspect several major reasons for the heterogeneous distribution of patients with ASD across regions in the country. The fickleness of clinical manifestations in individuals with ASD is a serious challenge in trying to make the correct diagnosis. In addition, there are neither physiological markers, cerebral correlates, genetic determinants, nor stable clinical criteria that would allow us to consider variants of mental development disorders as discrete entities. Therefore, there is a shift away from the nosological paradigm, when the “disease” is replaced by a “spectrum of disorders”. This approach to diagnosis is perceived by part of the psychiatrists’ community as a regress in clinical concepts [21]. The developers of the latest diagnostic classifications have to take into account the limitations of modern scientific knowledge in the evidence-based categorization of mental disorders. Therefore, to improve diagnostic reliability, it was decided to expand the unified criteria for the clinical assessment of autism. The diagnostic criteria used in the ICD-10, on the contrary, create prerequisites for discrepancies in the clinical assessment of developmental disorders and other psychopathological conditions. Thus, for example, the study by B.D. Mendelevich in 2008 established that in the Russian Federation, there is a 316-, 93-, 27-, and 88-fold gap in the incidence rates of organic mental disorders, schizophrenia, mild mental retardation, and other forms, respectively, by region in children under the age of 14 [22]. These data indicate the low reliability of diagnostics with existing clinical approaches in psychiatry. Patients and their families become victims of circumstances, being forced to change their place of residence in search of the “right” diagnosis and adequate care.
Opponents of the concept of ASD point to significant differences in the typology of these disorders, based on the principles of descriptive psychopathology and “psychiatry of the course.” This refers to the theoretical ideas of the last century regarding the procedural, organic or constitutional, and personality-based nature of autism. At the same time, to date, genetic anomalies or hereditary metabolic disorders as a cause of autism have, unfortunately, attracted the attention of psychiatrists to a much lesser degree.
In addition, representatives of the “old school” criticize the practice of diagnostic prioritizing of ASD in patients with co-occurring intellectual disability (ID). Indeed, in the case of co-occurring ID and autism, the DSM-5 and ICD-11 assume the diagnosis of ASD, with an indication of the level of the concurrent disorder of intellectual development. There are reasonable grounds for such an approach. Intelligence in ASD can be quite difficult to measure. Assumptions that social communication disorder and, in particular, motor stereotypes are a consequence of ID [23] have been refuted in scientific studies. Thus, the use of special interventions for children with intellectual disabilities contributes to the emergence of alternative ways of communication and additional opportunities for them to solve complex problems [24–26].
Another discussed problem is the diagnosis of comorbid conditions in ASD [27]. Autism and schizophrenia is the existence of alternative and even mutually exclusive diagnoses for many domestic psychiatrists [28]. Therefore, as the patient ages, the diagnosis of autistic disorder may still change to a diagnosis of schizophrenia.
Despite a significant amount of research describing not only schizophrenia, but also other mental disorders as comorbid conditions with ASD, such as attention deficit hyperactivity disorder [29, 30], obsessive-compulsive disorder [31], catatonia [32, 33], bipolar disorder [34, 35], and others, a double diagnosis is still met infrequently in the field practice of a Russian psychiatrist.
Studies show that the involvement of the pediatric service is necessary for early detection and diagnosis of ASD. Since 2019, following Order No.396n of the Ministry of Health of the Russian Federation of June 13, 2019, changes have been made to the Procedure for Conducting Preventive Medical Examinations of Minors, approved by Order No.514n of the Ministry of Health of the Russian Federation of August 10, 2017. According to paragraph 16 of the new edition of the procedure, as part of the preventive medical examination of children who have reached the age of 2 years, screening for the identification of a risk group of developmental disorders is carried out by conducting a survey of the children’s parents and an examination by a child psychiatrist of children included in the risk group for developmental disorders [36].
Introducing screening into routine medical practice has been proven to promote early detection of ASD and other developmental disorders, compared to a diagnosis based solely on the physician’s clinical intuition.
The incidence of autism diagnosis is higher in those regions where NGOs actively work with pediatricians and teach them screening procedures [37]. Thus, in the Voronezh region, 35.7 people with ASD under FU per 100,000 population were registered, which is above the 75th percentile.
However, in most regions, the involvement of the pediatric service in ASD risk screening remains unacceptably low.
The stigma associated with a psychiatric diagnosis also remains a serious problem that prevents timely access to psychiatrists and the identification of developmental disorders. It is important to note that the primary task of the psychiatric service after a diagnosis of ASD is to register the child with the medical, social, psychological, and pedagogical support system. In the absence of such a system being in place, the patient’s family does not see the benefit of consulting a psychiatrist. Assistance in choosing an adequate educational path and provision of a wide range of social services for patients with ASD is likely to facilitate early consultation with a psychiatrist.
Conclusion
Our study has shown significant (104.5-fold) differences in ASD diagnosis rates by regions in the country against a backdrop of a low (compared to international data) number of registered cases of autism. This suggests that, since a significant number of individuals with ASD do not appear for a diagnostic assessment timely, the diagnosis is delayed and this group of patients does not receive adequate medical, social, psychological and pedagogical support. The reasons probably include different approaches to diagnosing ASD, low involvement of the pediatric service in screening activities, and fear of stigmatization by way of a mental disorder in the absence of a developed, accessible infrastructure of medical, social, psychological, and pedagogical support for people with ASD. To identify such patients, it is necessary to include ASD screening in routine medical practice in all regions of the Russian Federation and record the diagnosis in statistical reporting forms. Further studies in the regions of the country are needed to identify the problems standing in the way of a timely diagnosis of patients with ASD, as well as efforts to develop comprehensive care based on the principles of evidence-based effectiveness.