Introduction
Physical illnesses are often accompanied by signs of stress and maladjustment, in the form of depressed mood and increased anxiety. It is reported that 18–33% of patients who have suffered a stroke also suffered from depression [1]; anxiety symptoms occur in 28% of non-psychiatric inpatients, and 8% meet the criteria for some anxiety disorder [2]. Affective symptoms and medical disorders have a compounding negative impact that manifests through psychological, behavioral, and physiological mechanisms. Anxiety and low mood may be a patient’s reaction to disease, and a negative assessment of the prospects for recovery may limit that patient’s usual activity and social circle; in turn, a physical illness can exacerbate the manifestations of an already existing mental disorder [3, 4]. Negative behavioral manifestations include addiction, sleep disorders, or violation of the treatment regimen [5]. Physiological mechanisms include increased inflammatory response and hypothalamic-pituitary-adrenal axis impairment [6]. Research also points to an association between anxiety disorders and hypertension [7]. Together, these factors can worsen the course and prognosis of the physical illness, reduce the effectiveness of treatment, and slow down recovery. Thus, the search for effective means of treatment of negative mental state is an important independent undertaking in the management of patients with physical illnesses.
The use of pharmacological resources for the treatment of comorbid symptoms of maladjustment, along with proven efficacy, has a number of limitations, such as an adverse increase in the pharmacological load; an often long period of effective dose selection; possible contraindications and side effects; and, for some drugs, the potential for addiction [8]. Non-pharmacological methods of treatment with comparable efficacy in such a context will have an advantage. Another traditional, and effective, form of care for various types of distress and maladjustment is psychotherapy. At the same time, data have been accumulating on the positive impact of different activities, such as meditation, yoga, various breathing practices, and mindfulness practices on the mental state [9, 10]. Literature suggests that meditation practices reduce stress levels and hypertension [11–13]. Studies also show that the regular use of meditation, relaxation, and breathing practices contributes to many positive changes in both the emotional state of those practicing them and aspects of their physical health, such as a significant reduction in stress hormones [14] and markers of chronic inflammation [15], as well as normalization of elevated blood pressure (BP) [16–19].
In an attempt to achieve a standardization and reproducibility of these types of care, investigators and professionals are increasingly turning to technologies that are based on virtual reality. Virtual reality (VR) is a simulated three-dimensional immersive environment in which the user can act according to prearranged scenarios [20]. In recent years, various VR applications have found increasingly wide application in medical practice, including programs for both specialists (training of specific skills, simulation of medical processes, etc.) and patients (relaxation and stress management, overcoming anxiety, neurorehabilitation, etc.) [21–23]. According to the results of these studies, VR-based applications show a level of efficacy comparable to that of pharmacological, and, sometimes, even superior efficacy as a treatment means for anxiety disorders [24], phobias [25], eating disorders [26], and other psychopathological conditions. Such data justify the attempts being made to transfer relaxation practices to high-tech platforms. VR technologies allow, on the one hand, to standardize the procedure, and, on the other hand, they do not rule out the possibility of customizing the scenario, taking the patient’s condition into account, selecting the optimal program duration, setting breathing parameters, preferred locations, as well as other parameters.
In Russia, Viartech Development LLC has developed the Flow relaxation program, integrated into a capsule chair, for people with various manifestations of a stress reaction, anxiety, or tension.
The main goal of this study was to evaluate the efficacy of the relaxation scenario in the VR Flow technology in relation to the symptoms of anxiety and asthenia in patients undergoing inpatient treatment. Study hypothesis: taking a course of sessions of a specially designed relaxation VR scenario, in addition to the primary therapy, should help reduce the severity of anxiety and affective symptoms.
Methods
Study design
The study used an open-label design with a comparison group and simple randomization.
Sample
The enrollment of study participants was carried out from March to June 2021 among patients of both sexes aged 18 to 68 years who were undergoing inpatient treatment at the Speech Pathology and Neurorehabilitation Center of the Moscow Healthcare Department.
The main inclusion criteria of the study were as follows:
— complaint of anxiety, bad mood, asthenia, tension, increased fatigue, and other manifestations of maladjustment;
— understanding of the study instructions and procedures, readiness and ability to sit through VR sessions, filling out of questionnaires and scales.
The exclusion criteria were as follows:
— severe cognitive, motor and/or speech impairments that prevent understanding of the instructions and limit one’s ability to follow the study procedures;
— diagnosed epilepsy or a history of convulsive seizures;
— diagnosed mental illness (bipolar disorder, major depressive episode, schizophrenia, schizoaffective disorder, etc.);
— severe, decompensated or unstable physical illnesses.
Enrollment and randomization
The study information leaflet informed the patients that it was not known in advance to which group (experimental or control) they would be assigned, and that that would be determined randomly. All patients in the comparison group could, if they so desired, undergo a course of VR after completing the program.
The participants were assigned to a particular group as follows: After inclusion of a new patient and the signing of an informed consent form, the clinical researcher called authors of the protocol who had no relation to the recruitment of patients in the study and did not come into direct contact with them. A randomization table was used to assign patients to groups; according to this table, each participant’s serial number was randomly assigned a code of one of two groups: 40 codes for the VR group and 20 codes for the comparison group. After the clinical researcher at the site had received the group code for a new participant, this information became open to everybody.
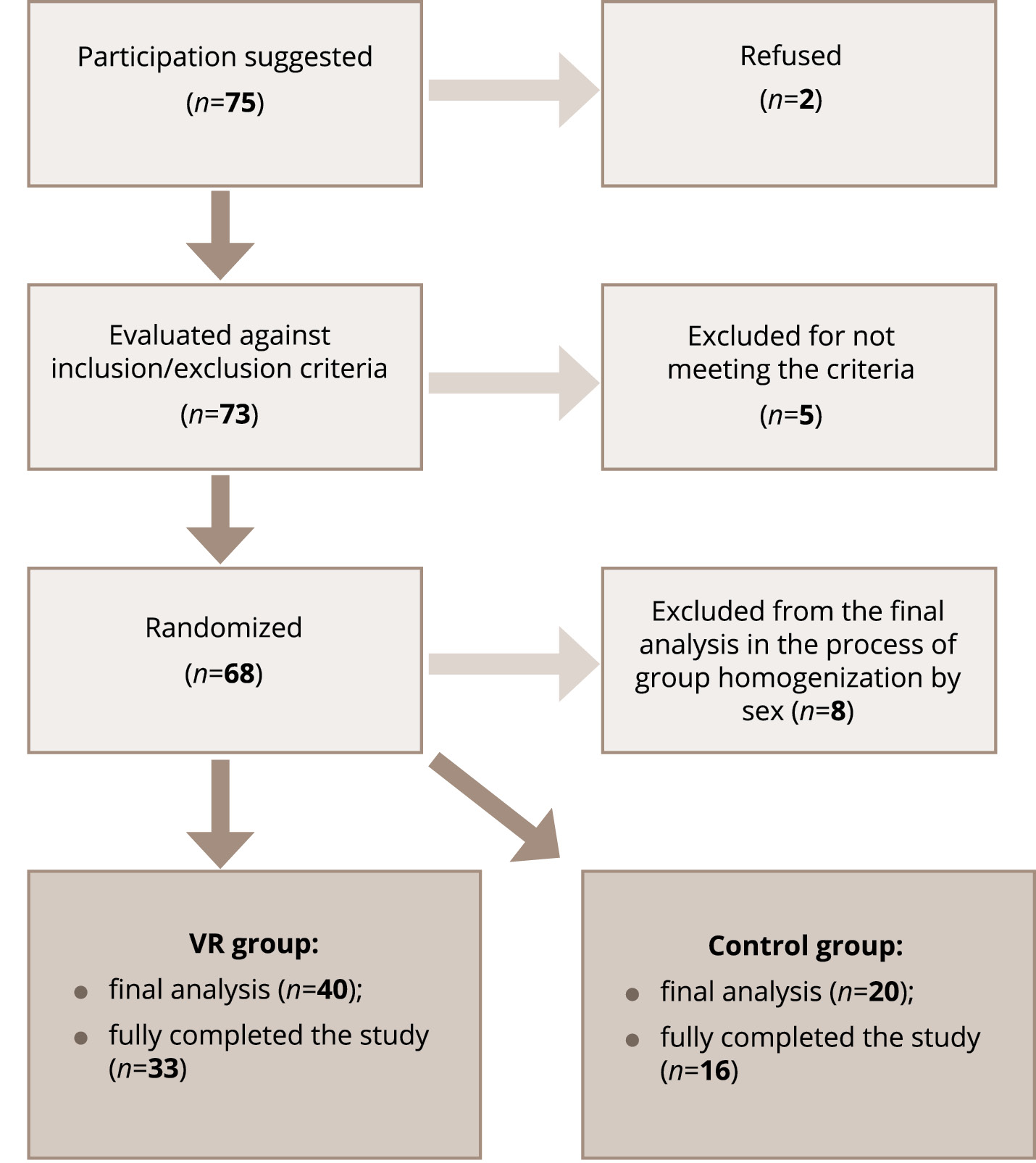
The enrollment continued until an equal ratio of male and female patients in each group was achieved; data from patients included at the end of the recruitment who did not meet the target 1 : 1 sex distribution were removed from the final analysis. In case of early withdrawal, the analysis included data collected at the time of exclusion. The primary ground for early withdrawal from the program was the end of hospitalization. The recruitment process is shown in Figure 1.
Figure 1. Participant flowchart.
Evaluation tools
The following procedures were used to assess the condition of patients:
- Spielberger State Anxiety Inventory [27]. This is a questionnaire to assess the severity of state anxiety (as opposed to anxiety as a personality trait), consisting of 20 statements that must be assessed on a 4-point scale. The procedure adaptation by Yu. L. Khanin provides the following indicative standards: 20–34 means a low level of anxiety, 35–44 means a moderate level of anxiety, and above 46 means a high level of anxiety.
- The Daily Fatigue Impact Scale (D-FIS) [28], consisting of 8 statements, was developed to assess the current state and daily changes in the symptom of fatigue associated with non-psychiatric illnesses. The patient rates each statement on a 5-point scale (0–4); a higher symptom severity corresponds to a higher total score.
- The Well-being, Activity, Mood (WAM) questionnaire [29] explores three aspects of the current psycho-emotional state indicated in the title. The subject is asked to correlate his current well-being with the scale assessment between pairs of words describing the poles of one state (for example, cheerful-gloomy, tense-relaxed). The result is separate scores on the subscales of well-being (WAM-W), activity (WAM-A), and mood (WAM-M); the 30–50 range is the average (normal) level for each of them.
- The Depression, Anxiety and Stress Scale (DASS-21) [30] is a questionnaire consisting of 21 statements to be ranked on a 4-point scale (0–3) for an assessment of the states of depression, anxiety, and stress experienced by the subject during the preceding week. The scale is not diagnostic; the concepts of stress, anxiety, and depression were used by the developers as a continuum to describe subjective experience. The final assessment in this test is the total score: the higher it is, the more pronounced the negative affective symptoms of the state.
All of these scales are self-questionnaires and are filled in by patients on their own.
Clinical Global Impression Scale-Severity (CGI-S) and Clinical Global Impression Scale-Improvement (CGI-I) [31] are filled in by the clinical researcher. These are 7-point scales in which the doctor is asked to assess the severity of the patient’s condition as a whole (at the first visit) and the changes in the patient’s condition (at subsequent visits) in comparison with other patients with a similar diagnosis based on their clinical experience.
Study procedures
Patients of the experimental group underwent a relaxation VR session on a daily basis for five days. Physical parameters (pulse rate) were measured before and after each session. Filling of the scales and questionnaires by the patient and patient’s condition assessment by the investigator were performed twice on the first day of the study (before and after the VR session), after the final (fifth, if the patient had not dropped out earlier) session, and five days after the end of the course. The total duration of the program thus amounted to 10 days (+2–5 days).
Patients in the control group underwent the same procedures, excluding VR sessions. On the first day, the interval between the first and subsequent measurements was about 6 hours.
All patients received standard pharmacotherapy, in accordance with the established diagnosis.
The following are the main outcomes of the study: the psychometric characteristics of patients in the experimental and control groups at the first examination; changes in the estimated parameters as a result of a single VR session, after a course of five sessions and long-term, as well as a comparison of these data with the results of the control group; assessment of the statistical significance of the changes in parameters for each of the groups; and data on changes in physiological parameters as a result of VR-relaxation.
Virtual reality scenario
All patients were given explanations about the upcoming VR sessions and their schedule by clinical researcher. To undergo the scenario, the patient was placed inside a specially equipped cocoon chair with a rotating bowl. Immediately before each relaxation session, the administrator of the VR capsule helped the participants to sit comfortably in the chair, fix the equipment (helmet, heart rate monitor), and provided support during the session.
The VR-program is a practice of guided relaxation, combining the methods of body therapy, hypnotherapy, work with negative emotional states and images. As part of the study, two virtual locations were used: a tropical beach and a mountainous landscape (Figure 2), which alternated uniformly for all participants in the study. The main characteristics that were taken into account when creating virtual locations were as follows: the practice space had to create a feeling of safety and comfort, be natural and at the same time cultivated, reflect the presence of the person in it, be filled and at the same time devoid of intense and stimulating elements that distract attention and interfere with focusing on internal processes. At the beginning and end of each session, the users assessed their state at the moment using a series of visual analog scales; they did this by placing a slider on these scales using the controller (joystick). The patients also noted the most pronounced emotions that they could detect in themselves at that moment. Depending on the assessments and responses of the patient, some stages of the practice were dynamically changed. Elements of scenario interactivity also included the ability to adjust some of the dynamic aspects of the scenario: the option to linger on one of the stages (for example, to better awareness of the ongoing processes), transition from one stage to the next.
Figure 2. Screenshots of Flow locations.
One session took an average of 20 to 30 minutes, depending on the characteristics of the state indicated by the patient at the beginning of the scenario, and the preferred speed of navigation within it.
Description and technical characteristics of the equipment
The following devices were used: a capsule chair for working in VR; a PC-based VR Oculus Rift S headset with built-in tracking; NZXT H1 650W computer with Intel Core i5-10600kf processor; Polar OH1 heart rate tracker; Samsung Galaxy Tab A7 32GB LTE (SM-T505N); Huawei e3372 modem.
Statistical analysis
The obtained primary data were analyzed using the statistical software package Statistica 6.0, version for Windows (StatSoft Inc.).
Mean values (M) and standard deviation (SD) were used when processing the results. Deltas (the magnitude of changes in psychometric parameters compared to the baseline) were studied to compare the degree of psychological changes in the experimental and control groups. The significance of the differences between the groups at different stages of the study was assessed using the Mann–Whitney test (p). The Wilcoxon rank sum test (p) was used to assess the significance of the changes in each of the groups during the study. Differences were considered significant at the level of р <0.05. The presence of a statistical relationship between the parameters was tested using the Spearman’s rank correlation coefficient (R).
Ethics
The study was approved by the ethics committee of the Speech Pathology and Neurorehabilitation Center of the Moscow Healthcare Department. Before participating in the study, all patients read the program information sheet and signed an informed consent form.
Results
The average age of the patients in the VR group (20 men and 20 women) was 44.8±15.9 years. The average age of the participants in the control group (10 men and 10 women) was 39.0±14.7 years. Differences in age between patients of the two groups were not statistically significant (p=0.19).
The study cohort consisted of patients with the following diagnoses (according to the International Classification of Diseases, 10th revision): 23 patients (38.3%) with stuttering (F98.5); 16 patients (26.7%) with other mental disorders due to damage to or dysfunction of the brain or due to physical illness (F06.x); 15 patients (25%) with personality and behavioral disorders due to illness, damage to and dysfunction of the brain (F07.x); 3 patients (5%) with sequelae of the COVID-19 coronavirus infection (U07.1) and other viral pneumonia (J12.8); 2 patients (3.3%) with somatoform autonomic dysfunction of respiratory organs (F45.38); and 1 patient (1.7%) with adjustment disorders (F43.2).
Baseline data
At the first examination, patients in both groups demonstrated an average level of state anxiety (Spielberger State Anxiety Inventory), a high and very high level of anxiety on the DASS-21 scale, and average scores on the WAM scale. Patients from the VR group had a higher degree of state anxiety symptoms, manifestations of depression, stress (DASS-21), fatigue (D-FIS), and also characterized their well-being, activity, and mood (WAM scale) lower. However, significant differences were observed only for two parameters of the WAM questionnaire (lower assessments of well-being (WAM-W) and mood (WAM-M) in the VR group) (Table 1).
Table 1. Results of the psychometric assessment of patients at the first measurement (baseline), M±SD
|
Scale |
Experimental group (VR) |
Control group |
Significance of differences, p |
|
Spielberger State Anxiety Inventory |
42.93±11.43 |
39.45±9.87 |
0.28 |
|
DASS-21 |
22.05±16.12 |
16.76±11.91 |
0.27 |
|
D-FIS |
12.05±9.31 |
7.01±4.29 |
0.22 |
|
WAM-W |
44.30±14.54 |
53.7±10.91 |
0.01* |
|
WAM-A |
42.50±11.89 |
47.9±10.94 |
0.08 |
|
WAM-M |
48.28±13.88 |
56.05±11.07 |
0.02* |
Note: The asterisk (*) marks the statistical significance of differences at р <0.05.
The average values of physiological parameters at the first measurement in the experimental group were as follows: systolic blood pressure, 124.87±11.62 mmHg; diastolic, 79.37±10.32 mmHg; pulse rate, 70.87±12.34 units.
Changes in scale parameters in the groups during the study (intergroup comparison)
A single VR session led to a significant improvement in the well-being and mood of patients according to the WAM questionnaire, and it also reduced depression, anxiety, and stress according to the DASS-21 scale. After the final session of the VR course and five days after, the patients showed statistically significant positive changes in all studied psychometric parameters (Table 2).
Table 2. Values of the scale parameters at time of visits and significance of changes (p) compared with the first measurement in the VR group, M±SD
|
Scale |
First measurement (before the first VR session) |
After the first VR session |
р |
After a course of five VR sessions |
р |
5 days after completing the VR course |
р |
|
Spielberger State Anxiety Inventory ↓ |
42.93±11.43 |
40.83±9.6 |
0.94 |
39.05±9.45 |
0.006* |
38.54±8.99 |
0.026* |
|
DASS-21 ↓ |
22.05±16.12 |
19.46±15.69 |
0.04* |
16.9±11.9 |
0.01* |
14.18±11.72 |
0.009* |
|
D-FIS ↓ |
12.05±9.31 |
10.65±8.62 |
0.33 |
8.0±5.27 |
0.003* |
6.94±4.76 |
0.006* |
|
WAM-W ↑ |
44.30±14.54 |
47.51±14.37 |
0.01* |
50.53±11.4 |
0.007* |
51.67±12.52 |
0.003* |
|
WAM-A ↑ |
42.50±11.89 |
44.41±12.87 |
0.89 |
47.05±10.1 |
0.03* |
49.67±9.12 |
0.0008* |
|
WAM-M ↑ |
48.28±13.88 |
50.33±13.58 |
0.04* |
53.03±10.05 |
0.015* |
54.09±10.2 |
0.023* |
Note: The asterisk (*) marks the statistical significance of differences at р <0.05; The arrows (↓) show the direction of the positive changes in the parameter.
In the control group, patients did not show significant changes in the studied parameters compared with the baseline assessment, with the exception of the DASS-21 score by the fifth day of the study. The table of average scale parameter values in the comparison group and the significance of the changes at the time of each visit is given in Table S1 in the Supplementary.
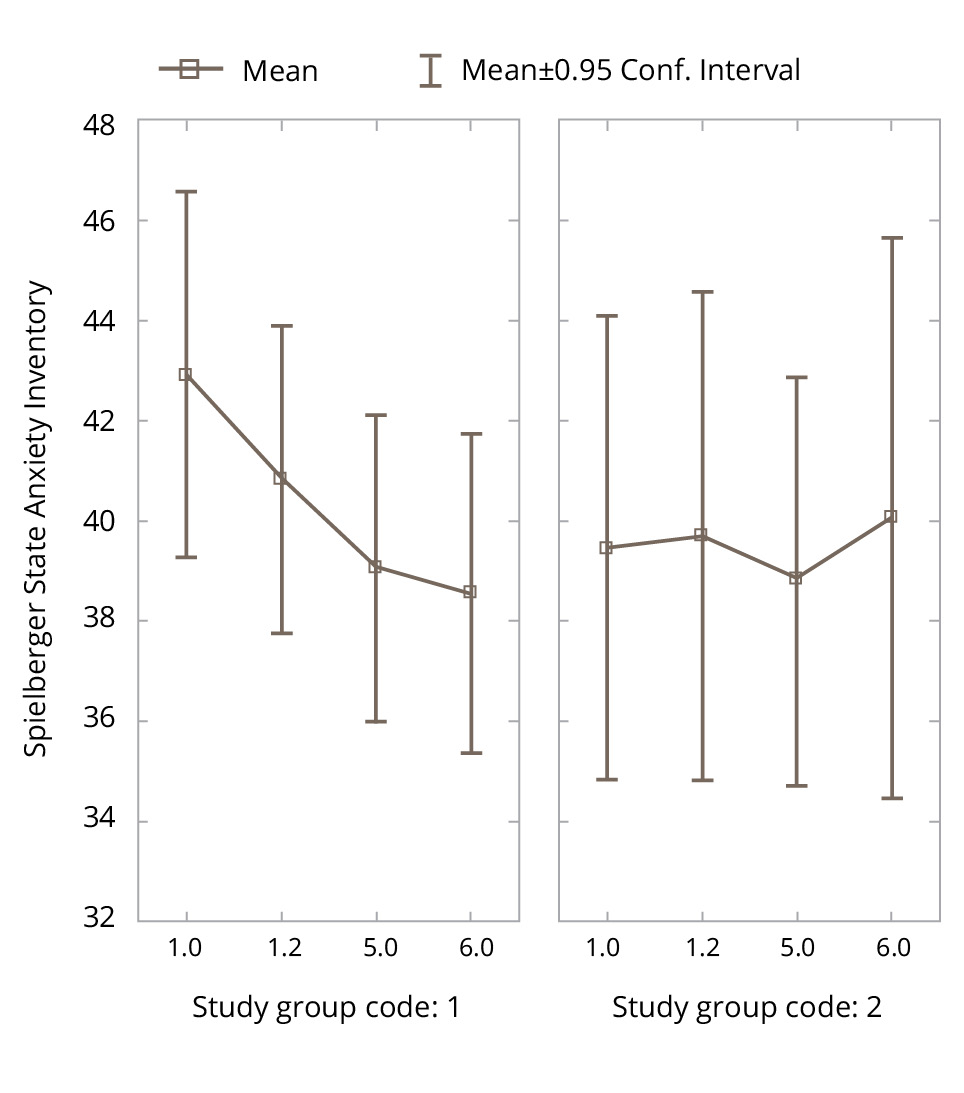
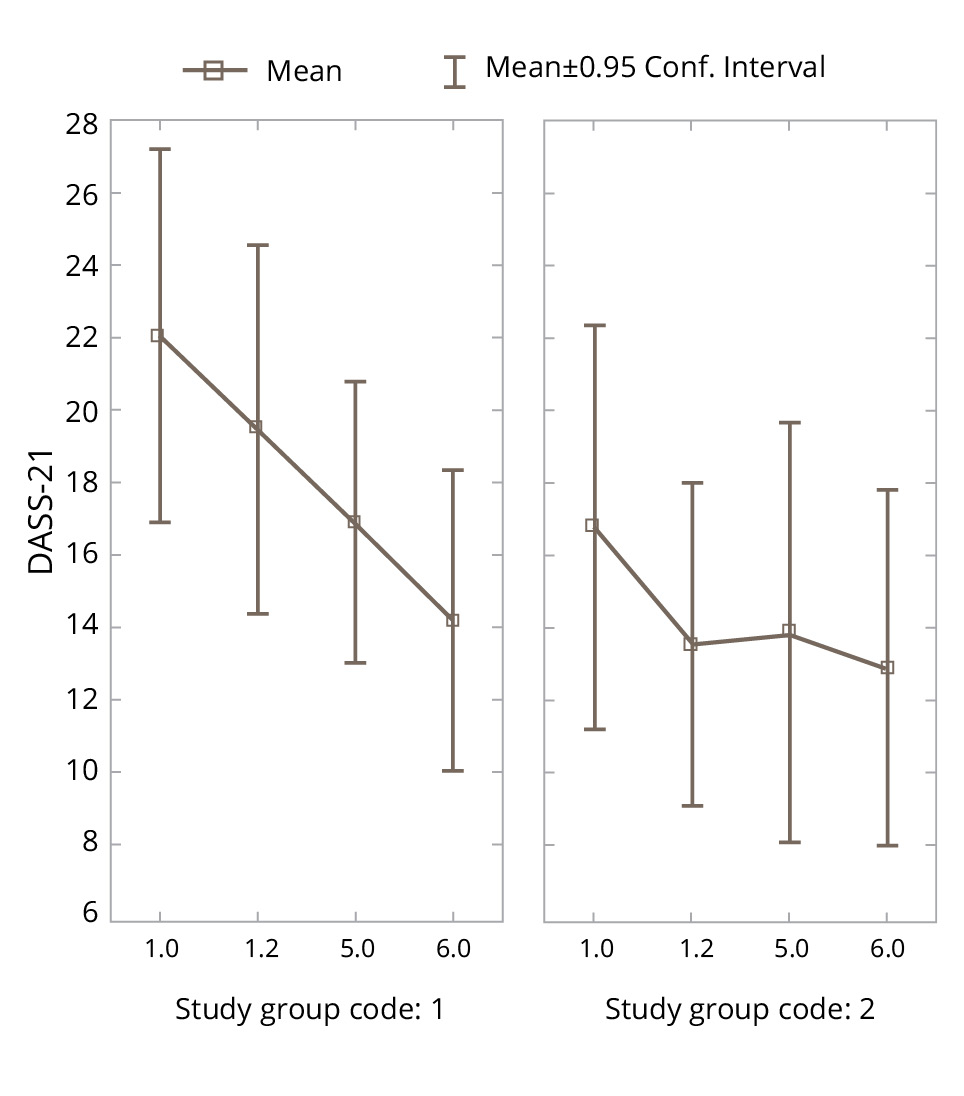
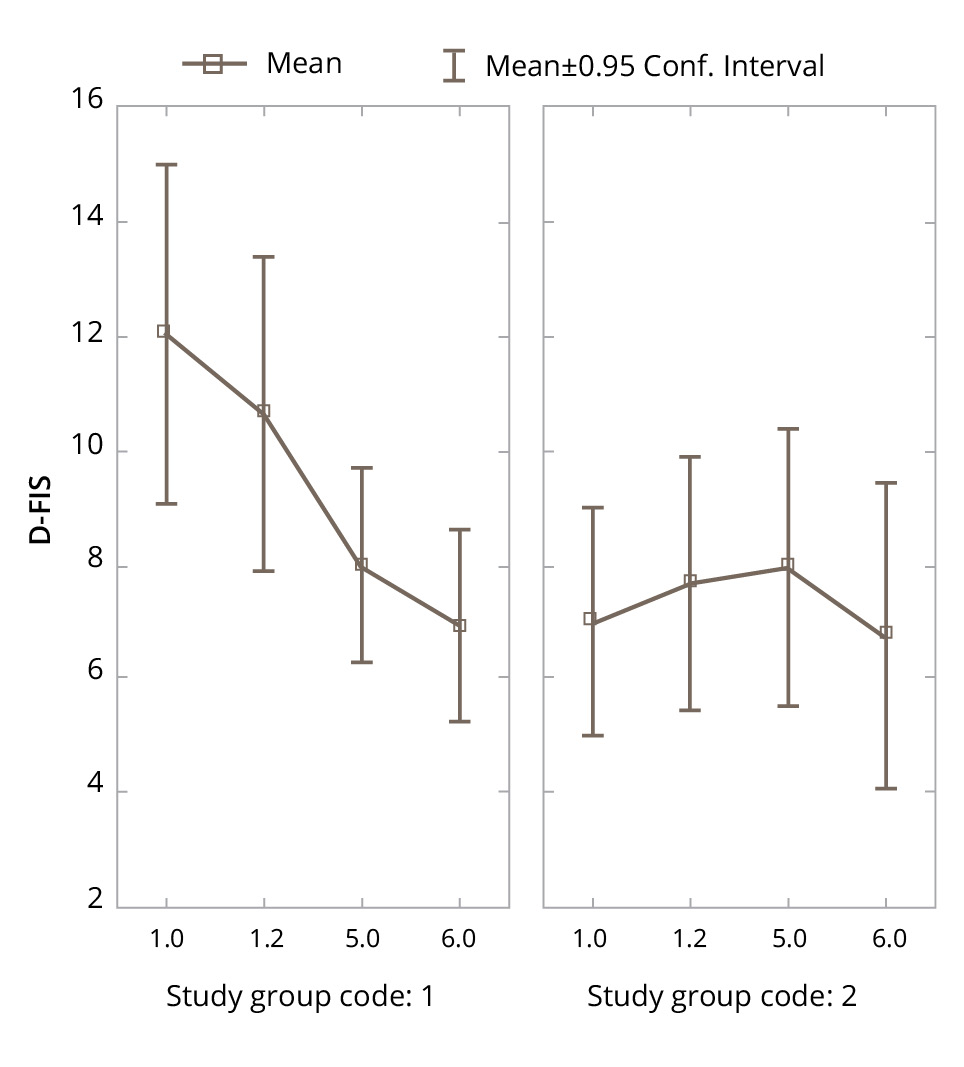
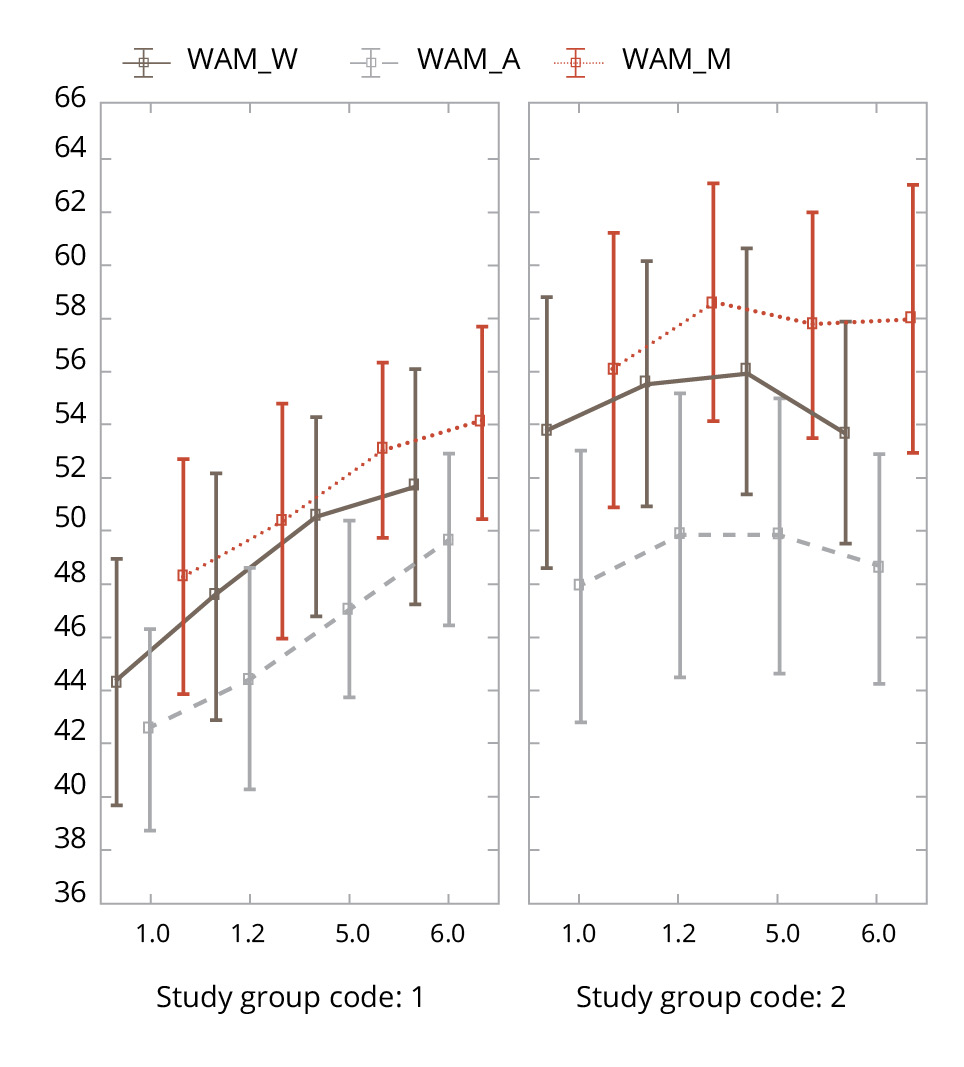
The dynamics of the studied parameters in the experimental and control groups during the study is graphically presented in Figures 3–6.
Figure 3. Changes in the Spielberger State Anxiety Inventory parameters in the experimental and control groups during the study. Note: Designations here and in Figures 4–6: group code in study 1 — experimental group (VR), group code in study 2 — control group; 1.0 — baseline examination, 1.2 — assessment after the first VR session, 5.0 — assessment after a course of five VR sessions, 6.0 — assessment 5 days after the completion of the course of VR sessions in the experimental group and the corresponding points in the control group.
Figure 4. Changes in the DASS-21 parameters in the experimental and control groups during the study.
Figure 5. Changes in the D-FIS parameters in the experimental and control groups during the study.
Figure 6. Changes in the WAM parameters in the experimental and control groups during the study.
Comparison of the degree of changes in psychometric parameters (intragroup changes)
Changes in the psychometric parameters compared to their baseline (delta) during the study in the experimental and control groups are presented in Table 3.
Table 3. Changes in psychometric parameters and the significance of differences (p) between them in the experimental and control groups during the study, M±SD
|
Scale |
First day |
Fifth day |
Long-term |
|||
|
VR group |
Control group |
VR group |
Control group |
VR group |
Control group |
|
|
Spielberger State Anxiety Inventory |
–2.1±7.36 |
0.1±4.56 |
–3.82±7.55 |
–0.65±6.73 |
–3.67±8.02 |
–0.38±6.31 |
|
р=0.262 |
р=0.194 |
р=0.14 |
||||
|
DASS–21 |
–2.0±5.36 |
–0.06±4.38 |
–5.03±10.42 |
–2.84±5.67 |
–5.58±11.26 |
–1.56±6.93 |
|
р=0.256 |
р=0.883 |
р=0.466 |
||||
|
D–FIS |
–1.4±4.6 |
1.0±3.78 |
–3.9±6.89 |
0.95±3.89 |
–3.73±6.68 |
0.006±4.44 |
|
р=0.167 |
р=0.023* |
р=0.123 |
||||
|
WAM-W |
3.26±7.52 |
0.05±6.37 |
5.95±13.05 |
2.3±5.39 |
6.85±13.89 |
–1.63±6.21 |
|
р=0.191 |
р=0.173 |
р=0.0034* |
||||
|
WAM-A |
1.92±7.26 |
–0.11±5.73 |
4.24±13.06 |
1.9±7.99 |
6.67±9.9 |
–0.69±5.9 |
|
р=0.185 |
р=0.279 |
р=0.014* |
||||
|
WAM-M |
1.59±4.6 |
0.39±4.09 |
4.71±11.04 |
1.7±8.44 |
4.88±11.28 |
0.5±6.06 |
|
р=0.389 |
р=0.19 |
р=0.207 |
||||
Note: The asterisk (*) marks the statistical significance of differences at р <0.05.
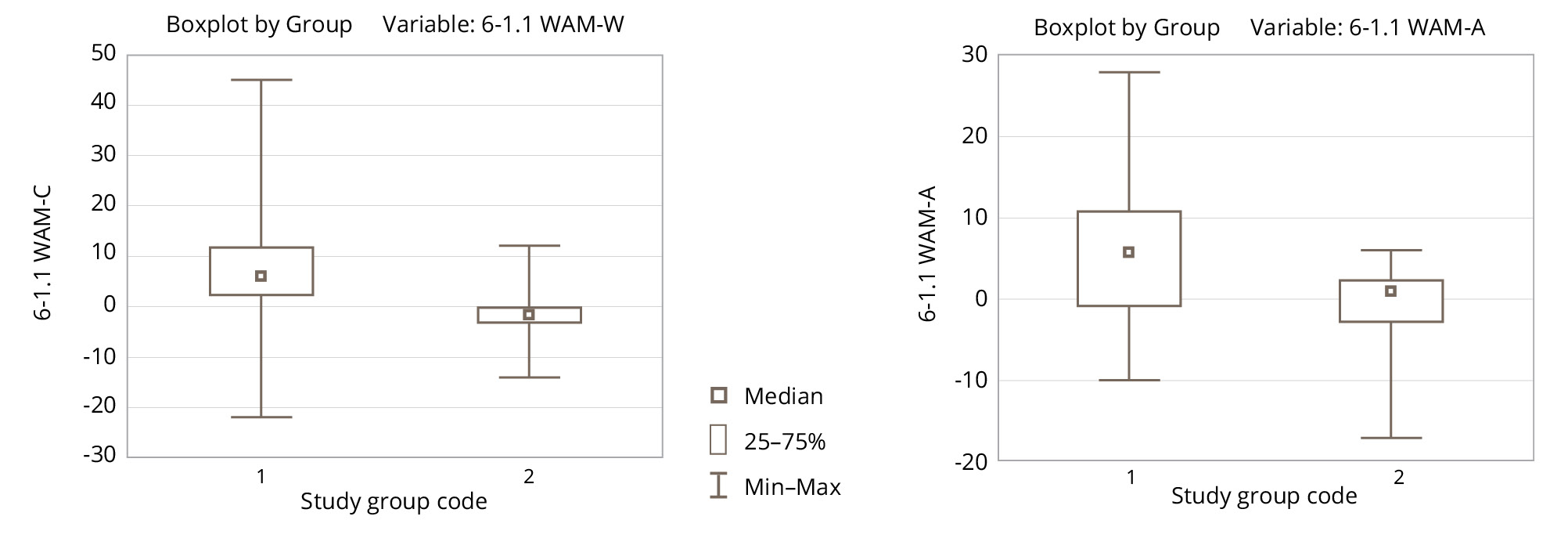
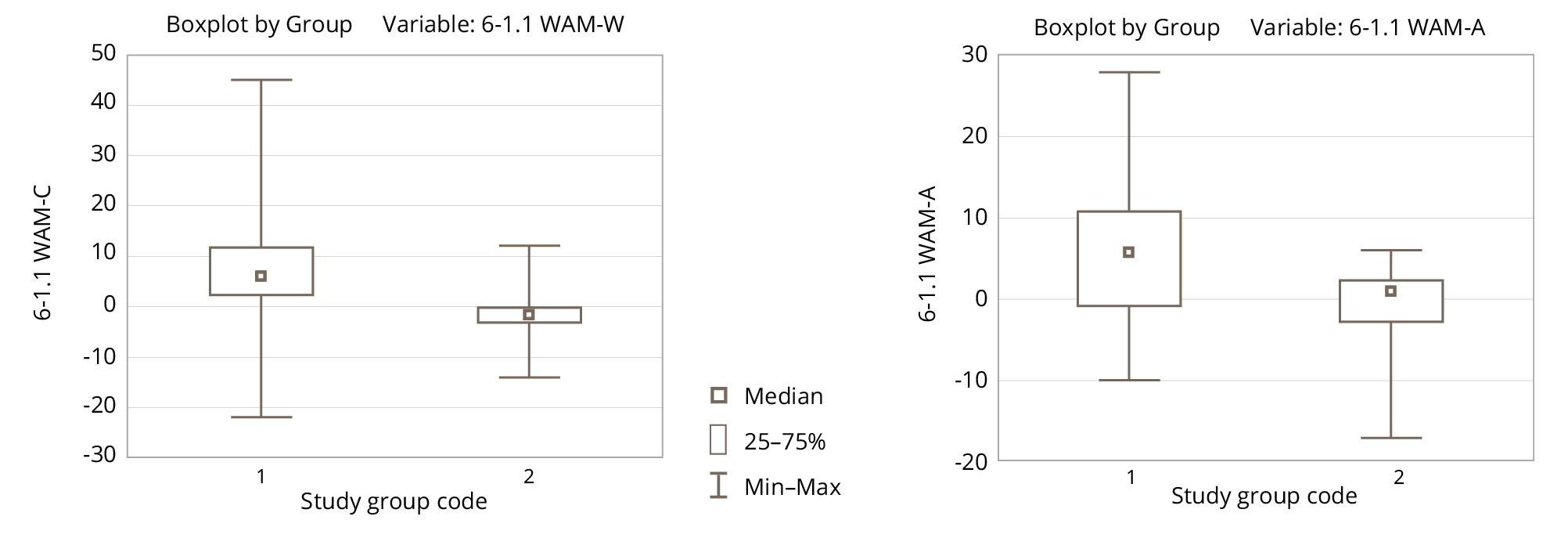
On the first day, there were no significant differences between the groups in terms of the changes in psychometric parameters; however, by the fifth day, significant differences were visible in the D-FIS score (severity of the fatigue symptom): a more pronounced reduction in the symptom was observed in the group of patients who had undergone a course of relaxing VR sessions (Figure 7).
Figure 7. Changes in the D-FIS score between the first measurement and on the fifth day in the experimental (1) and control (2) groups. Note: The D-FIS score is an inverse scale: higher values mean greater symptom severity, so the lower the delta (visit 5 minus visit 1.1) the better.
At the follow-up visit (five days after the completion of a course of five VR sessions), the experimental group showed significantly more pronounced positive changes according to the WAM questionnaire in terms of well-being and activity (Figure 8).
Figure 8. Changes in the WAM scale parameters between the first measurement and the final measurement in the experimental (1) and control (2) groups.
Changes in physical parameters as a result of sessions of virtual reality
One of the objectives of the study was to investigate changes in the physical parameters (blood pressure and pulse rate) as a result of undergoing VR-relaxation. The average values of systolic, diastolic blood pressure and pulse rate before and after undergoing VR sessions are presented in Table 4 (after the first session) and in Table S2 in the Supplementary (after the second and subsequent sessions).
Table 4. Blood pressure and pulse rate before and after the first VR session (n=40) and the significance of changes (p), M±SD
|
Stage |
Blood pressure, mm Hg |
Pulse rate, units |
|
|
systolic |
diastolic |
||
|
Before the session |
124.87±11.62 |
79.37±10.32 |
70.87±12.34 |
|
After the session |
120.03±13.05 |
76.68±9.23 |
68.21±9.66 |
|
р |
0.0008* |
0.016* |
0.0002* |
Note: The asterisk (*) marks the statistical significance of differences at р <0.05.
There is a significant decrease in all parameters in most cases as a result of undergoing the VR program. The decrease in blood pressure was more pronounced in individuals with initially higher blood pressure. In a subgroup of 11 such patients at the final VR session (5 patients with high-normal blood pressure according to the World Health Organization classification of hypertension, 4 patients with grade I hypertension, 2 patients with grade II hypertension), the decrease in blood pressure was even more pronounced (Table 5).
Table 5. Blood pressure before and after the fifth VR session and the significance of the changes (p) in the subgroup of patients with elevated and high blood pressure (n=11)
|
Stage |
Blood pressure, mm Hg |
|
|
systolic |
diastolic |
|
|
Before the session |
140.55±9.35 |
86.64±6.47 |
|
After the session |
124.63±11.96 |
80.27±12.23 |
|
р |
0.003* |
0.02* |
Note: The asterisk (*) marks the statistical significance of differences at р <0.05.
It was also found that for patients with a systolic pressure of 130 or higher before the first VR session, a more pronounced blood pressure decrease after the VR session (at the first visit) meant more pronounced changes on the Spielberger State Anxiety Inventory; i. e., patients with high blood pressure simultaneously showed a reduction in both BP and anxiety (R=0.52).
Discussion
Main findings
The conducted study provides empirical confirmation of the efficacy of the VR relaxation scenario for patients with anxiety and bad mood in a hospital setting. Comparison of the psychometric parameters of patients who underwent a course of VR sessions with patients from the control group shows a clear advantage in terms of positive changes in the first group. There is a significant benefit that accumulates and remains after the completion of the course in terms of improvement regarding anxiety, fatigue, bad mood, various aspects of well-being in the VR group, while patients in the control group showed no significant changes in these parameters throughout the entire study period. The psychological benefit of VR sessions was also reflected in the physiological parameters: blood pressure and pulse rate. Interestingly, the more pronounced the disorders at the beginning of the study were, the more significant the improvement in the patients’ condition in terms of both their mental status and autonomic disorders proved.
Strengths and limitations of the study
This study was the first study of the efficacy of the VR relaxation scenario Flow in a clinical sample. The positive aspects of the study also include the significant number of participants in the program, sufficient psychometric tools for pilot testing of the hypothesis put forward, and the presence of a comparison group. The study design allowed us to investigate the effects of not only a single VR session, but also the whole course, as well as the stability of the achieved improvement in patients. The limitations of the study are the clinical heterogeneity of the studied cohort of patients, the lack of consideration of the diagnosis impact and the contribution of the pharmacotherapy received by the participants to the observed changes.
Comparison with the existing literature
A wide review of VR studies [32] published between 2000 and 2020 and indexed in major electronic databases (a total of 28 studies analyzed) confirms the effectiveness of using various programs based on VR technology for the treatment of many negative mental conditions, including post-traumatic stress disorder, specific phobias, and social anxiety.
A number of systematic reviews highlight the application of VR methods in a hospital setting. VR instruments have been shown to be effective in relieving pain and reducing preoperative anxiety in adult patients [33], as well as in a group of adolescent patients [34].
It should be noted that a significant portion of meta-analytical studies using VR technologies do not distinguish between the content of the software, taking into account both virtual games and 3D trips and programs developed specifically for certain therapeutic tasks, although it would seem reasonable to expect the effectiveness of the latter to be higher. In this sense, a direct correlation of the results of various studies may be, to some extent, incorrect from a methodological point of view.
The positive aspects of VR technology also usually include its good tolerance by patients, a high level of involvement of participants, and the possibility of reducing the drug load [35, 36]. Wide introduction of the technology at this stage is limited by the rather high cost of equipment and, to a greater extent, the lack of proven tools for solving specific therapeutic problems and the high costs of their development.
In general, the results of this study are consistent with those of other studies, which also show that the use of tools based on VR technology is effective in addressing various manifestations of anxiety and psychological distress.
The positive results obtained from the Flow pilot study allow us to be optimistic about the prospects of the VR platform in both clinical and outpatient practice. There could be future studies on other samples (including clinical ones) or new scenarios developed within the platform.
Conclusion
The results of this study show that the use of the VR relaxation scenario Flow is an effective and promising tool for reducing anxiety and affective symptoms in non-psychiatric inpatients and can be recommended for inclusion in a care program in medical institutions.