Posttraumatic Stress Disorder (PTSD) is a chronic and disabling condition affecting 5–10% of the U.S. general population [Kessler, 2005] and approximately 3.9% in cross-national samples [Koenen, 2017] (see Table 1 for diagnostic criteria). It is associated with high rates of both psychiatric and medical disorders. For example, people with PTSD are more likely to experience mood disorders, anxiety disorders, substance use disorders, chronic pain, and cardiovascular disease [Alonso; Beckham, 1997; Kessler, 2005; Toomey, 2019]. PTSD is also associated with significant problems in relationships, early retirement and job loss, and diminished quality of life [American Psychiatric Association; Bleich A, Solomon, 2004; Gueze, 2009; Yu, 2016].
Rates of PTSD are higher for military veterans (ranging from 10–25%) compared to the general population [Kang, 2003; Kuester, 2017; Kulka, 1990]. A number of factors have been shown to increase the risk for PTSD in military veterans, including younger age, racial minority status, lower socioeconomic status, higher number of deployments, prior emotional problems, and lack of social support [Reisman, 2016]. Moreover, military or combat-related PTSD may be more difficult to treat than civilian PTSD [Goodson, 2011; Levi, 2021]. For instance, studies have found large non-response rates among military and veteran populations [Forbes, 2010], high drop-out rates [Schnurr, 2022], and smaller treatment effect sizes [Bisson, 2007; Bradley, 2005]. That said, there is still a large effect size for evidence-based psychotherapies in combat veterans (d=1.2, [Goodson, 2017]).
The PTSD treatments with the greatest empirical support are Prolonged Exposure Therapy and Cognitive Processing Therapy. Prolonged Exposure is a behavioral based therapy with strong empirical support for military related PTSD [Eftekhari, 2013; Goodson, 2017; Schnurr, 2022]. The standard Prolonged Exposure protocol is usually around 12 sessions in military veterans [Goodson, 2013] and has 4 major components: 1) psychoeducation about trauma and PTSD; 2) breathing retraining; 3) in vivo exposure; and 4) imaginal exposure.
Cognitive Processing Therapy is arguably the most used therapy across the United States Veteran Health Administration System, and it has a large body of empirical support [Reisman, 2016; Resick, 2016]. Cognitive Processing Therapy is based on the theory that trauma related beliefs and interpretations (also known as cognitive “stuck points”) maintain PTSD symptomology. These stuck points are either assimilated (changing the event to take responsibility or blame on self) or over-accommodated (rigid all-or-nothing beliefs about the world or others). Cognitive restructuring interventions are used to increase awareness about trauma-related thoughts and eventually challenge trauma-related beliefs (stuck points; [Resick, 2016]).
Building on Existing Treatments — Behavior Therapy for Anxiety and PTSD
Both Prolonged Exposure and Cognitive Processing Therapy are empirically supported treatments for PTSD in military populations with a strong empirical foundation. However, they are not without limitations. First, these therapies can require considerable time, financial, and personnel resources to implement. For example, standard Prolonged Exposure trainings are 4 full days followed by approximately 6 months of individual and group supervision (weekly). This a time consuming and costly proposition which often does not result in continued implementation by providers. For example, in one large urban Veteran Administration center, only 20% of 45 licensed providers continued to practice Prolonged Exposure after completing the initial training [Goodson, 2020].
Further, these therapies can be difficult for patients to fully understand and implement on their own. For example, cognitive interventions for PTSD require a patient to learn to identify automatic thoughts, evaluate their veracity, and then generate new cognitions. This highly deliberate and effortful restructuring process needs to be taught, practiced, and ultimately performed at times when the therapist is not there to help. Further, patients often need to complete the restructuring process during times of heightened emotions and high stress, when cognitive resources are even further diminished [Haeffel, 2019]. Another limitation is that the exercises used, and content discussed, in these treatments are emotionally arousing and highly distressing (e.g., repeated imaginal exposure). Thus, it may not be surprising that these therapies have drop-out rates ranging from 16% to 54% [Eftekhari, 2013; Jeffreys M.D, 2014; Kehle-Forbes, 2016; Schnurr, 2022]. Finally, recent findings have suggested that hypervigilance (along with sleep) are the least likely symptoms to respond in empirically-based principles treatments for PTSD [Cox, 2021].
To address these limitations, we created Behavioral Therapy for Anxiety and PTSD (BTAP), which is a simple, behavior-based therapy rooted in learning theory. Building on empirically established therapies such as Prolonged Exposure, BTAP has a singular focus on identifying, reducing, and countering safety behaviors that maintain PTSD. Because it only focuses on safety behaviors, it is simple to learn and implement; therapist trainings are one day, and follow-up consultation provided as needed.
What Are Safety Behaviors?
“Safety behaviors” are actions and mental processes that people engage in to avoid feared outcomes [Salkovskis, 1991]. They manifest in a variety of forms ranging from excessive reassurance seeking to frequent handwashing. The use of safety behaviors can be adaptive, and even necessary, in the presence of actual threat such (such as being hypervigilant during combat). However, in the absence of actual threat, the use of safety behaviors has been associated with negative outcomes, particularly increases in anxiety [Deacon, 2008; Fawzy, 2015; Goodson, 2016; Olatunji, 2011]. Studies show that reducing safety behaviors enhances treatment outcomes across anxiety disorders [Kim E.-J, 2005; McManus, 2008; Morgan, 1999; Wells, 2016]. For example, a meta-analysis by Heibig-Lang and Petermann [Helbig-Lang, 2010] found that the efficacy of exposure therapy could be increased by reducing safety behaviors. Similarly, failure to address safety behaviors results in smaller treatment gains [Helbig-Lang, 2014; Sloan, 2002] and the reemergence of anxious symptoms after treatment [Beesdo-Baum, 2012]. Surprisingly, despite the inclusion of safety behaviors in early conceptualizations of PTSD [Dunmore, 1999], no clinical interventions have examined the effect of reducing and countering safety behaviors on symptoms of PTSD. In PTSD, common safety behaviors include: vigilance (e.g., scanning others for danger) suppression (e.g., pushing away trauma memories, keeping mind occupied, distraction), checking (checking doors/windows are locked), escape/evade (leaving situations early), avoidance/withdrawal (lack of engagement in situations and activities), worry/rumination (excessive planning, analyzing traumatic events), and safety bolstering (e.g., safety aids such as guns) [Goodson, 2021].
In the sections to follow, we describe the BTAP manualized treatment (available on the Open Science Framework: https://osf.io/z38qv/), provide case examples and report preliminary support for its effectiveness in military veterans.
BTAP Protocol
BTAP has four treatment phases: 1) assessment, 2) education, 3) safety behavior reduction related to intrusive imagery (e.g., suppression of trauma memories), and
4) safety behavior reduction related to threat and anxiety (e.g., vigilance). An optional fifth phase is focused on safety behavioral reduction related to trust, withdrawal, and rumination. We provide case-example information and preliminary treatment data on 5 BTAP cases. All cases were veterans diagnosed with PTSD and treated on a VA PTSD Clinical Team.
Phase 1: Assessment
Patients are first administered baseline assessments of safety behavior usage and PTSD symptoms. We use the Safety Behavior Assessment Form (SBAF; [Goodson, 2016]) and the PCL-5 (PTSD Checklist for DSM-5; [Weathers, 2013] for these purposes, respectively (available on Open Science Framework: https://osf.io/z38qv/). The SBAF assesses safety behaviors in a wide variety of anxiety and trauma-related conditions; it consists of 6 subscales: PTSD, vigilance, generalized, social, panic, and health. The PTSD subscale consists of 12 common PTSD safety behaviors that are frequently targeted in BTAP. However, assessment for additional safety behaviors is crucial as many are ideographically related to patient fears (see BTAP manual available on Open Science Framework for lists of safety behaviors not covered by the SBAF). A few core safety behaviors may be added to the PTSD subscale for each patient (although these additions are not included in the total score). The PTSD subscale, along with the PCL-5, are used to track progress in treatment across sessions.
Case Example. Adam was an Iraq veteran in his 30s’ with a PTSD diagnosis. He was administered the SBAF and scored high on the PTSD subscale as expected (mean item score of 2.3; range is 0-3) endorsing items such as scoping places out before entering, sitting with back to wall, watching others for signs of danger, and checking locks on doors and window. These items were recorded as safety behaviors he might choose to try to eliminate. He also scored high on the social anxiety subscale (mean item score of 2.3) endorsing items such as monitoring conversations, monitoring others’ reactions, preparing what to say ahead of time, and hiding anxiety. Based on this information, the therapist probed for a possible comorbid Social Anxiety Disorder and found that Adam did indeed meet criteria. In discussing treatment goals, it was agreed to incorporate a small number of social anxiety safety behaviors to address in treatment (self-monitoring, prolonging conversations, etc.).
Phase 2: Education (Sessions 1–3)
Phase two is dedicated to socialization and teaching patients about safety behaviors. The first session involves socialization to treatment, assessing motivation, and establishing treatment goals and expectations. For example, the client is informed that he or she will be expected to do homework on a daily basis. Likewise, he or she is told that safety behavior practices will often necessitate going places specifically to practice the exercises, and that it will not be possible to complete this treatment without any changes to one’s routine. Additionally, it is explained that self-report measures will be completed each session and discussed. Finally, the patient is introduced to the two major phases of treatment
(i.e., safety behavior reduction related to intrusive imagery and safety behavior reduction related to threat and anxiety) and he or she selects which one with which to begin.
After socialization, the beginning sessions are dedicated to education about safety behaviors including: a) what they are, b) how they maintain PTSD symptoms, c) how to monitor them, and d) how to reduce/eliminate them. Additionally, patient’s major safety behaviors are identified along with corresponding fears or beliefs, as well as how these have maintained the patient’s symptoms over time. A corresponding client workbook helps solidify the education provided in treatment (available on Open Science Framework: https://osf.io/z38qv/).
Finally, monitoring is carried out. This includes identifying safety behaviors in real time as well as the fear or negative belief driving each safety behavior identified. Identified safety behaviors and corresponding negative beliefs or fears are recorded to consider for elimination. In addition, a behavior experiment designed to identify safety behaviors is included as an optional monitoring component; patients engage in a challenging situation for the purposes of eliciting safety behaviors. Upon completion of the education and monitoring phase, all major safety behaviors should be identified. The list of safety behaviors (from questionnaires, in-person queries, and monitoring) is called the “master list”; it should contain approximately 10–20 safety behaviors to be addressed in treatment.
Case Example. Don is a married, White, male in his 70’s who was a highly successful career service member. He was experiencing PTSD symptoms. After socialization, Don was given information about the temporary nature of anxiety and trauma and factors that cause them to become chronic. First, it was explained that trauma memories are unprocessed (i.e., unfinished business) which results in continued intrusions and high levels of associated distress. The intrusive memory and related negative emotions result in safety behaviors. The session ended with two homework assignments: 1) read chapters 1 and 2 from the safety behavior client workbook; and 2) monitor safety behaviors using the “Where, What, Why” safety behavior monitoring form (available on Open Science Framework: https://osf.io/z38qv/).
Phase 3: Intrusive Imagery Safety Behaviors (Sessions 3–7)
This phase consists of four primary components. The first component is the elimination of safety behaviors related to intrusive memories (e.g., distracting oneself, and not talking about the traumatic memory). Patients are asked to eliminate these safety behaviors in conjunction with the following three strategies:
1) Acceptance of Intrusive Memories and Related Feelings: This safety behavior elimination strategy begins with education about the paradoxical effects of memory and emotion suppression. Following, acceptance of intrusive memories is introduced, taught, and practiced in-session (“Welcoming Intrusions”). Specifically, patients are instructed to recall intrusive images and then recognize their bodily sensations and feelings. For homework, patients are asked to practice in-the-moment acceptance when intrusions occur as well as carrying out Welcoming Intrusions for 15 minutes per day. In-the-moment acceptance of intrusions is considered a core skill and is practiced throughout all of treatment.
It should be noted that one of the most common safety behaviors in PTSD is keeping oneself (and mind) busy. To reduce this safety behavior, the patient should be asked to conduct an experiment in which he or she does nothing for 30 minutes. Distressing thoughts or memories should be written down in a journal. Following, the patient should be instructed to spend certain periods of time each day doing nothing (this can be presented as opportunity to practice in-the-moment acceptance).
2) Purposeful Trauma Recall: This is a safety behavior countering strategy that naturally follows intrusion acceptance practice. In this countering strategy, the trauma is slowly walked through with images being identified for each major scene of the trauma. Following, the patient is asked to recall and hold each image and fully accept (“lean into and embrace”) the feelings. This exercise typically takes 20–30 minutes and the patient is asked to practice each day.
3) Written Trauma Exposure: This is a safety behavior countering strategy in which the patient writes a narrative about the trauma. Throughout the writing process, the therapist periodically asks the veteran to stop and feel his or her feelings. Upon completion of the written exposure, the veteran reads the narrative to the therapist. In between sessions, the patient reads the narrative each day and when new details emerge, he or she is asked to add them to the end of the narrative. The next week the trauma narrative is written again, and the new details are added. This practice continues until the patient feels he or she is “done” with the memory and no longer needs to read it.
Case Example. Cedric is a married, White, male who suffered a military related traumatic event that has “haunted” him for years. The first strategy used was in-the-moment acceptance. Cedric was asked to recall the trauma (no further specific instruction) and hold the image(s) for a few seconds. He was then asked to focus his attention on his body and fully feel whatever sensations or emotions arise for 20–30 seconds. This was practiced three times and given as homework practice. It was also emphasized that this intervention would continue to be practiced throughout all of the treatment.
The next intervention was the purposeful trauma recall. Cedric and the therapist walked through the major scenes and identified corresponding images. He was then asked to sequentially move from scene to scene and “hold” each image and “fully feel” any and all emotions that surfaced. This was completed 5 times in-session. Cedric found it somewhat difficult but did not foresee any problems carrying it out as homework. When Cedric returned the next session, he reported that he felt much less bothered by the memory and was ready to move to the next phase of treatment.
Phase 4: Threat and Anxiety Safety Behaviors (sessions 7–12)
Phase 3 is focused on reducing vigilance and anxiety-related safety behaviors and increasing self-efficacy. Initial strategies are geared towards reducing and countering vigilance, which are then followed by addressing threat and anxiety safety behaviors.
Vigilance is a safety behavior that lends itself to being dropped in all-or-nothing terms, as opposed to individual components. Whenever possible, we recommend practicing in-session. The initial task is to identify approximately 5–10 challenging “practice situations”. Next strategies for countering vigilance are discussed and the specific method or methods that will be used are agreed upon. Following, practices are carefully planned out in session, including the situation, the duration, the number of practices, the countering strategy, and any problems that may come up. Daily practice is encouraged with practices being at least 20 minutes in duration. We have found it helpful to meet the patient outside of the office and have one practice session together. This allows the therapist to provide real-time coaching with respect to dropping vigilance.
Vigilance practices should be continued as homework until: 1) the patient feels confident in his/her ability to drop vigilance; and 2) anxiety in situations has reduced. In debriefing practices, discussions emphasize what was learned and what still needs to be learned. Examples of methods for dropping or countering vigilance are listed in the manual.
Other anxiety and threat-related safety behaviors are addressed during this phase. For example, if the veteran frequently checks that doors are locked or does perimeter checks, they can be asked to delegate this activity to their spouse. If the veteran avoids situations or withdraws from important activities they can be asked to systematically engage in meaningful activities and counter avoidance. If the veteran leaves situations early, he or she can be asked to postpone leaving for an agreed upon amount of time. If the veteran ends conversations early, he or she can be asked to continue with conversations until they are ended by the other partner. If the veteran overly plans activities, he or she can ask their child or partner to select an activity and immediately embark upon it. If the veteran carries a gun, then he or she can be asked to go on outings without the weapon. It is very important that all practices are debriefed with an emphasis on what was learned and self-efficacy.
Often times in debriefing practices, underlying fears or negative beliefs associated with safety behaviors are processed. In fact, countering strategies can directly target underlying fears or beliefs. For instance, if the veteran holds the belief that no place is safe, he or she can be asked to enter into crowded situations and expose their back to others or sit at a coffee shop and read a paper or book. If the veteran believes that no one can be trusted they can ask others for favors, or put themselves in situations where they are reliant on others, or share information about themselves.
Clinical examples can be used to elucidate the emphasis on learning and underlying fears/beliefs. In a recent case, the first author assigned a veteran to walk downtown and not scan and then ride the city Tracks up and down main street without engaging in vigilance. In debriefing the practice, the veteran was asked what he learned. In response, he stated: “Well first-of-all, nothing bad happened… but also, that I’ll probably have an idea ahead of time if something bad is going to happen.” In a second example, a veteran with fears of losing control was asked to enter into a difficult situation and “do nothing” for an extended period of time. In debriefing the exercise, the veteran talked about his growing confidence in his ability to handle difficult situations and strong feelings.
Case example. Jose is a 40-year-old Afghanistan combat veteran. He retired from the military approximately one year prior to initiating BTAP. Jose was referred to BTAP after reporting little success with Cognitive Processing Therapy. The first session of the Threat and Anxiety Phase began with a review of the treatment rationale and his master list of safety behaviors to identify those safety behaviors to be addressed. Jose chose to practice dropping vigilance safety behaviors using Recognize, Drop, and Refocus (RDR) as the countering strategy. Specifically, agreed to go to Walmart for 30 minutes of vigilance dropping practice.
In the next session, Jose reported that he lasted only 1 minute and quickly abandoned the RDR technique when his anxiety escalated. Jose was praised for the one minute he was able to complete. That minute was referred to as the most important minute of treatment until this time. This is consistent with the “no failure” approach to BTAP. As long as an effort is made, the practice is considered a success. Jose and his therapist also processed what was learned in the experiment and were able to identify two important factors. First, Jose needed to start with some easier safety behaviors, and second, practices with his wife are more difficult. Jose was then asked what safety behaviors he would like to work on for the following week. He picked one safety behavior: not avoiding taking trails while hiking. The following session, Jose reported success with the practices. He noted that even though at times he felt like he was in Afghanistan, he was able to stay with the practice.
The following week, he selected two safety behaviors to address: 1) reducing contingency planning and 2) reducing perimeter checks. Jose returned the next session and reported feeling more depressed and stated he had not done much homework. He attributed this to not getting along with his wife. Again, Jose was praised for practicing at all, given he was in conflict with his wife and feeling more depressed. Some time was spent processing the marriage issue and then the focus was returned to BTAP.
Jose spent three more sessions in this treatment phase. He completed the following safety behavior practices: letting people walk behind him, saying hi to more people, talking with his neighbors more; and engaging in more social-public related activities. Jose had an excellent response to treatment.
Preliminary Effectiveness Data for BTAP
Participants were five male veterans (Mage=50; SDage=15.6) with PTSD treated on a PTSD Clinical Team (the vast majority of the veterans treated on this team are male). The majority of the participants were White (80%), with one being Asian-American. 8% had previous treatment for PTSD. Measures of PTSD symptoms, depression, quality of life and PTSD-related safety behaviors were administered pre and post, with the measures of PTSD and safety behaviors administered every session to track progress. All participants were seen weekly or twice weekly over telehealth. Patients were seen over telehealth due to COVID precautions. The average number of sessions was 10 (SD=2.9).
Measures
PTSD Symptoms. The PTSD Checklist (PCL-5), a 20-item self-report measure was used to assess the severity of PTSD symptoms [Toomey, 2019]. The PCL-5 is frequently used in VA settings and has good psychometric properties [Weathers, 2013]. Total scores range from 0–80 with higher scores indicating greater severity of PTSD symptoms.
Depressive Symptoms. The Patient Health Questionnaire-9 (PHQ-9, [Kroenke, 2001]), a 9-item self-report measure, was used to assess symptoms of depression. The diagnostic validity and high levels of sensitivity and specificity for major depression have been demonstrated for the PHQ-9 in several studies [Kroenke, 2001]. Higher scores indicate greater depression severity.
Quality of Life. The Behavioral Health Questionnaire–20 (BHQ-20, [Kopta, 2002]), a 20-item self-report measure was used to assess global mental health. The BHQ-20 has been found to be reliable and valid with adequate internal consistency, test-retest reliability, and construct validity [Kopta, 2002]. Two subscales (Wellbeing and Life Functioning) were used to assess Veterans’ quality of life. Scores from both subscales were summed for a total quality of life score, with scores ranging from 0–28.
Safety Behaviors. Safety behaviors and PTSD-specific safety behaviors were measured with Safety Behavior Assessment Form [Goodson, 2016]. The SBAF has been shown to have excellent psychometric properties across several different populations [Goodson, 2016] and is associated with anxiety and PTSD treatment outcomes [Goodson, 2018]. Higher scores indicate greater use of safety behaviors.
Results
As shown in Table, there were significant reductions in PTSD symptom scores over the course of treatment. The mean symptom reduction across the 5 veterans was 31 points, which corresponded to an effect size of 1.7 (Cohen’s d). Veterans also reported a significant reduction in the use of PTSD-related safety behaviors (mean 10-point reduction and effect size of 2.2). They also reported significant reductions in depressive symptoms (average reduction of 5.4 points and a corresponding effect size of 1.6). Finally, quality of life scores increased and had large corresponding effect sizes, but the pre-post difference did not reach significance, likely a result of low power. Figures 1–3 show session by session change for the primary study variables over the course of treatment.
Table
The diagnostic and statistical manual for mental disorders (DSM-5) criteria for PTSD
|
Intrusion Symptoms (1 needed for diagnosis) |
|
1. Unwanted, intrusive memories 2. Distressing recurrent nightmares 3. Flashbacks 4. Emotional reactivity when reminded of the traumatic event(s) 5. Physical reactivity (strong physical symptoms) when reminded of the traumatic event(s) |
|
Avoidance Symptoms (1 needed for diagnosis) |
|
1. Avoidance of distressing memories, thoughts, or feelings related to the traumatic event(s) 2. Avoidance of situations, places, activities, and people and cause reminders of the traumatic event(s) |
|
Negative Alterations in Cognition and Mood Symptoms (2 needed for diagnosis) |
|
1. Inability to remember important aspects of traumatic event(s) 2. Negative beliefs about self, others, or the world 3. Distorted thoughts of blame or responsibility about the traumatic event(s) 4. Persistent negative emotional states 5. Decreased participation in significant activities 6. Feelings detached or cut-off from others 7. Inability to experience positive emotions |
|
Alterations in Arousal (2 needed for diagnosis) |
|
1. Irritable behavior and angry outbursts 2. Reckless or self-destructive behavior 3. Hypervigilance or being overly watchful and on-guard 4. Exaggerated startle response 5. Concentration problems 6. Sleeping disturbance |
Notes. DSM-5 criteria differ from DSM-4 criteria in several ways. First, in DSM-5 PTSD is no longer considered an “anxiety disorder”, but rather it is now a “trauma-related disorder.” Second, DSM-5 expanded what constitutes a trauma, resulting in broader definition [Dunmore, 1999; Eftekhari, 2013]. Criteria related to the need to respond to the event with fear, helplessness, or horror was eliminated, but now includes: 1) being exposed to the aftermath of traumatic events; and 2) being informed of the sudden, violent death of a loved one [Dunmore, 1999; Eftekhari, 2013]. Finally, the DSM-5 changed the structure of the diagnostic criteria from 3 clusters (i.e., re-experiencing, avoidance/numbing, and arousal) to 4 clusters (i.e., intrusions, avoidance, negative alterations in cognition and mood, and alterations in arousal). The new diagnostic criteria include a total of 20 symptoms that are organized by cluster.
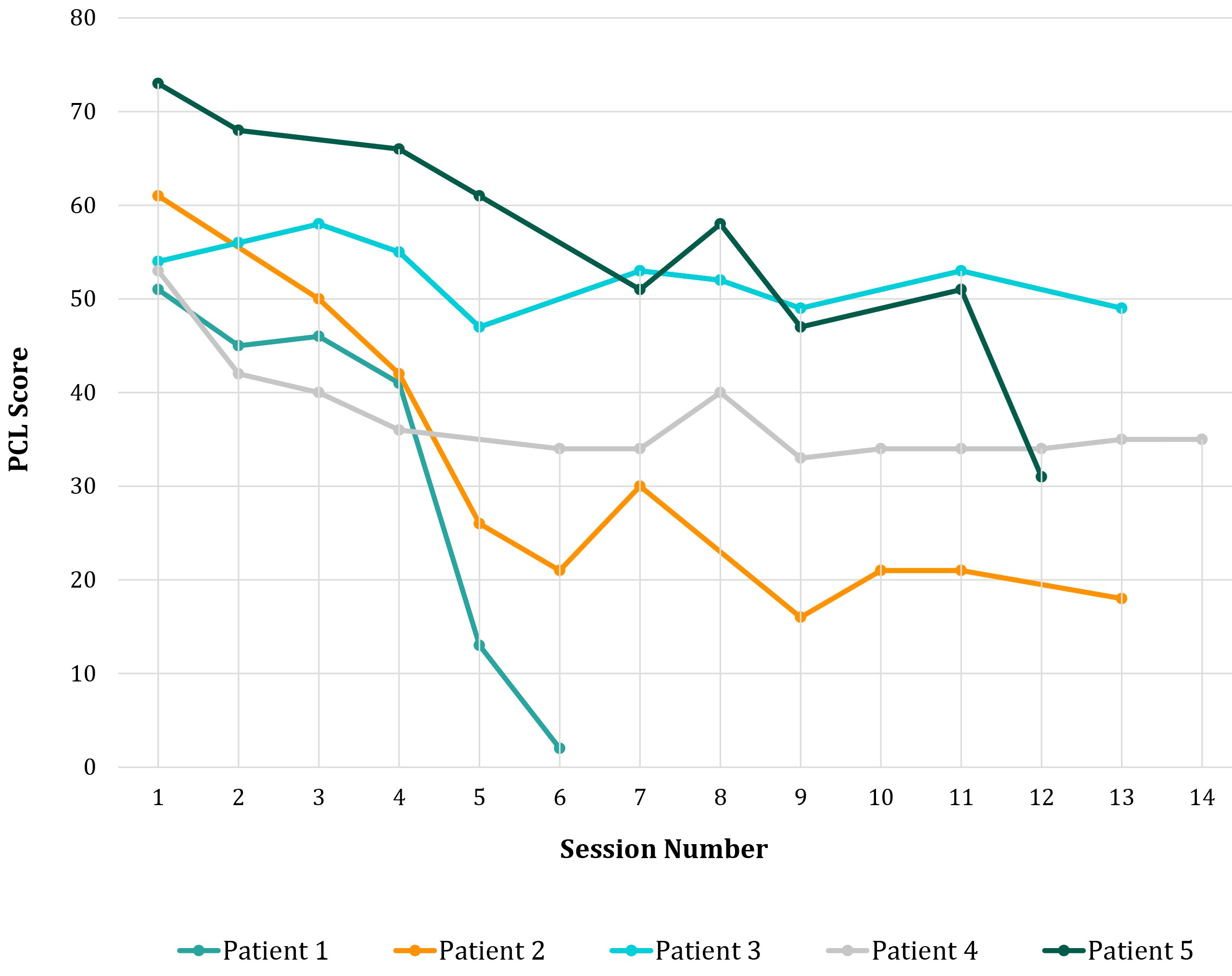
Figure 1. PTSD symptom scores over the course of treatment
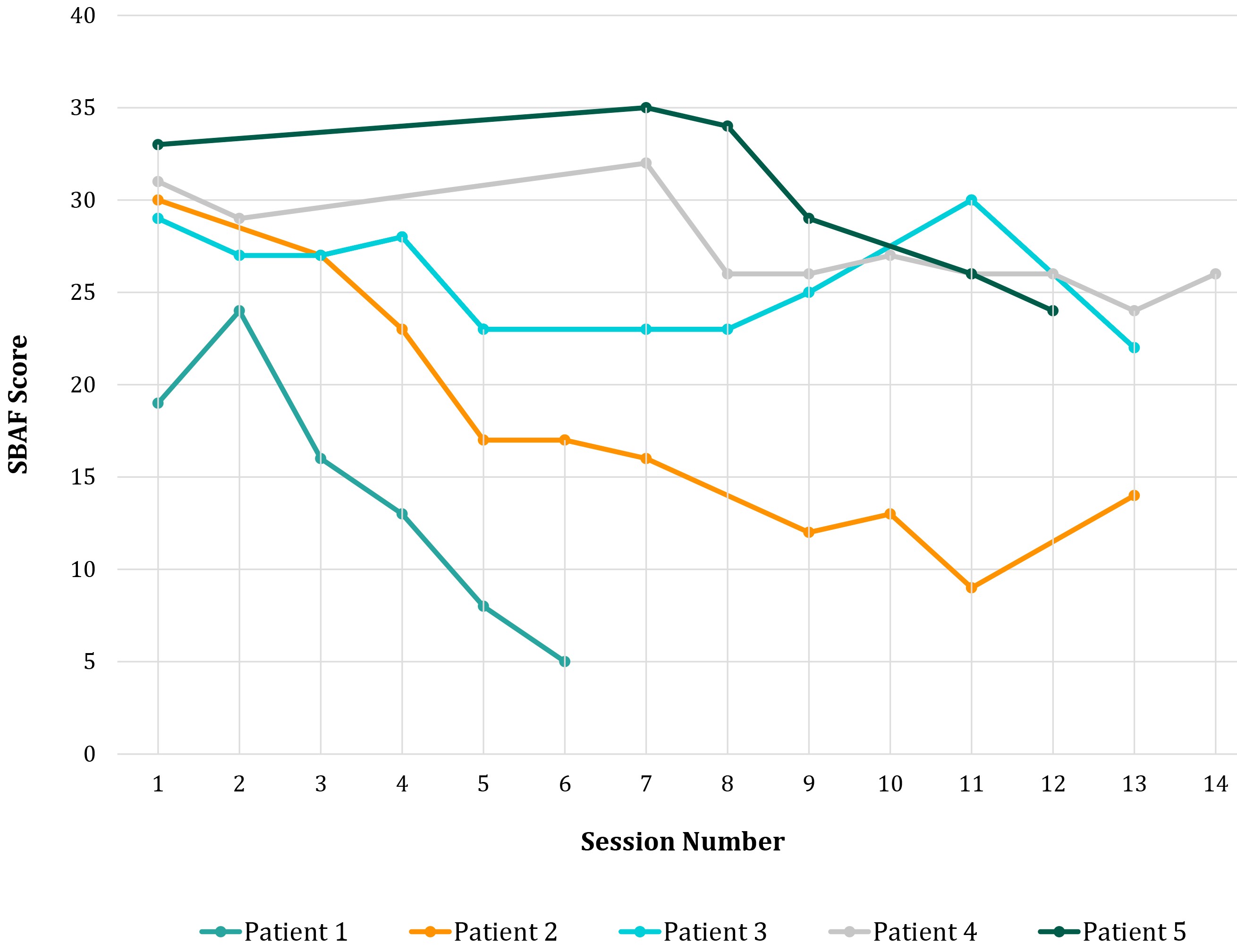
Figure 2. Safety behavior scores over the course of treatment
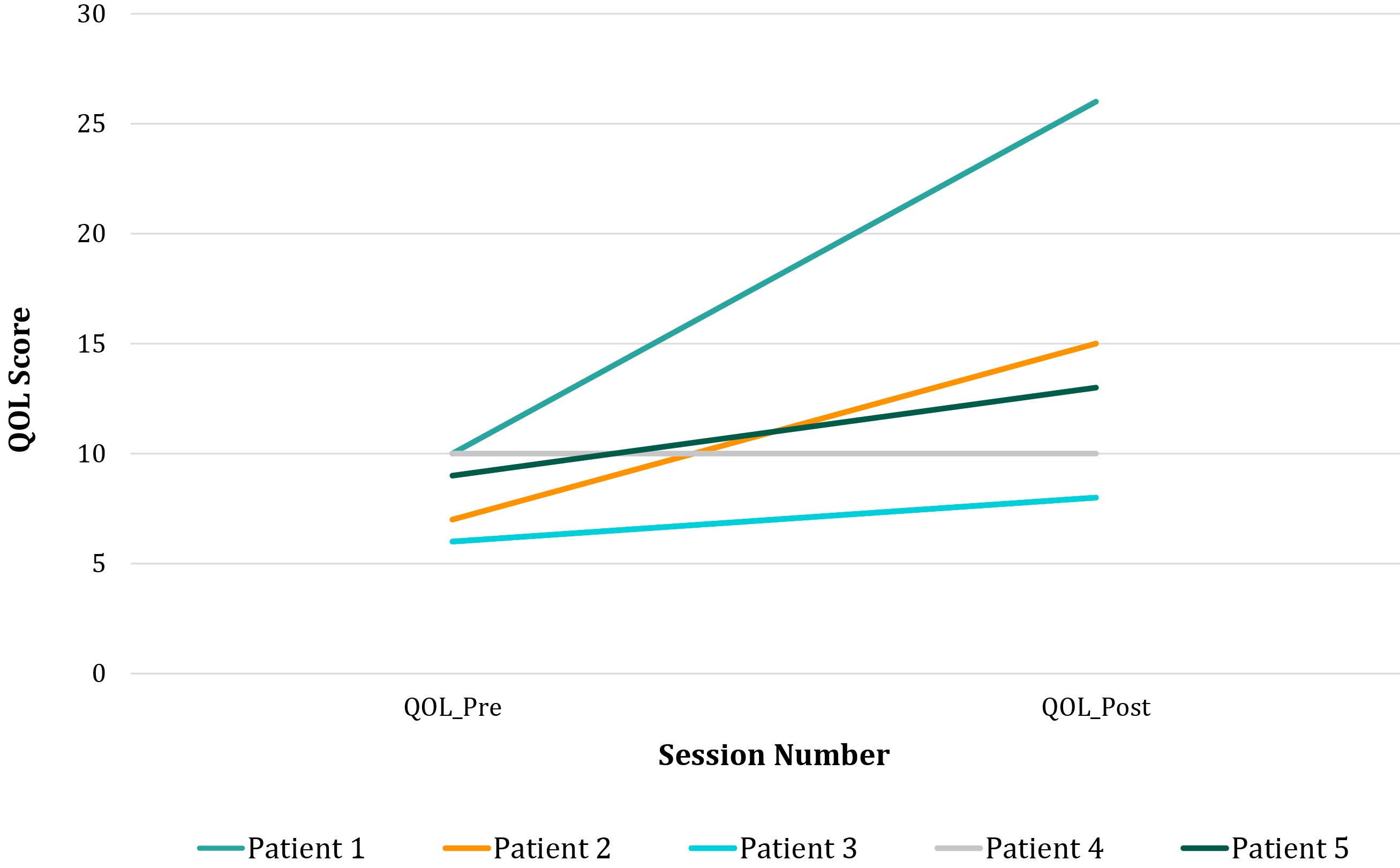
Figure 3. Quality of life and wellbeing scores over the course of treatment
Discussion
The purpose of this article was to provide a primer for using BTAP to treat PTSD in military veterans. We described the major treatment components, provide case examples, and preliminary effectiveness data. The preliminary outcomes from these 5 cases are encouraging and suggest that additional study of the effectiveness of safety behavior elimination as a treatment for PTSD is merited. All materials are on Open Science Framework, and thus, available to use in future research.
There are several theoretical reasons that support our preliminary effectiveness of BTAP for PTSD. First, as conceptualized by Ehlers and Clark [Ehlers, 2000], PTSD is a disorder of ongoing threat. It is well established in the research literature that safety behaviors both preserve and reduce threat. As such, addressing safety behaviors in PTSD is a sound conceptual fit with etiological models of PTSD development and maintenance. Second, vigilance is a difficult symptom to address and like worry, often is accompanied with positive and negative beliefs. A recent PTSD treatment study with veterans found vigilance (along with sleep) to be the least responsive to existing evidence-based treatments [Cox, 2021]. The existing treatments for PTSD to not directly target vigilance in the same rigorous way as BTAP. Indeed, most participants had several preferred vigilance strategies and without practice identifying and countering them, they would have remained intact, and the veterans at risk for relapse of symptoms [Beesdo-Baum, 2012]. BTAP is also promising in its simplicity. Most veterans easily grasp the concept of safety behaviors and bought into the rationale that reducing/countering safety behaviors would reduce symptoms of PTSD. For example, one veteran stated “I now have a set of tools for dealing with anxiety and PTSD that I can continue to use on whatever happens to come up.” This represents buy-in and the realization that safety behavior reduction is a successful strategy for dealing with anxiety and trauma in general. Lastly, BTAP is unique in its flexibility, which is likely highly desirable for trauma survivors. Veterans are given their choice of what safety behaviors to address, how to address them, and in what order they should be addressed. This flexibility likely enhances the therapeutic alliance which is also facilitates positive treatment outcomes. In fact, one veteran who had not responded to Cognitive Processing Therapy, stated that this treatment worked for him because: “I didn’t feel I was being told what I had to do or think.”
Although the results of this study are promising, the small number of participants is a limitation. Many treatments are shown to be effective in preliminary phases, but when the rigors of scientific methodologies are applied, their effectiveness dampens. Additionally, the study sample was all male and mostly White veterans. This lack of diversity should be taken into consideration before assuming generalization to more diverse populations. Likewise, the mean age of the sample was 50 and thus does not speak to the potential effectiveness with younger participants. However, these results do suggest that further study of safety behavior elimination to treat PTSD is merited.