Clinical Psychology and Special Education
2022. Vol. 11, no. 2, 196–206
doi:10.17759/cpse.2022110212
ISSN: 2304-0394 (online)
Proposing a Model-Based Addition of Risk and Protective Factors to the Evaluation of Displaced Youth
Abstract
Immigrant youth displaced from their homes are at great risk for developing emotional and behavioral symptoms and, therefore, they often present for assessment services in school, medical, and justice settings. The aim of this report is to describe unique, evidence-based risk and protective factors for psychopathology relevant to this client group including risk factors at the individual, family, and community levels that occur during premigration, perimigration, and postmigration. Adding assessment of these factors to a solid foundation of evidence-based assessment will enhance the breadth and depth of psychodiagnostic evaluations of immigrant youth. Protective factors, particularly family relationships, school connections, and peer support, must also be considered, as protective factors can be used to provide recommendations for services and interventions that capitalize upon existing sources of resilience. In addition to presenting a conceptual model and reviewing common risk and protective factors in the extant literature, this report closes with sample measures that can be quickly and easily added to an existing psychodiagnostic battery in order to tailor the assessment to immigrant youth.
General Information
Keywords: assessment, immigrant, adolescent, displaced youth, evidence-based
Journal rubric: Scientific Discussions
Article type: scientific article
DOI: https://doi.org/10.17759/cpse.2022110212
Received: 08.06.2021
Accepted:
For citation: Venta A.C. Proposing a Model-Based Addition of Risk and Protective Factors to the Evaluation of Displaced Youth [Elektronnyi resurs]. Klinicheskaia i spetsial'naia psikhologiia = Clinical Psychology and Special Education, 2022. Vol. 11, no. 2, pp. 196–206. DOI: 10.17759/cpse.2022110212.
Full text
Youth who are displaced from their home countries due to regional violence, persecution, and economic hardship has been the subject of widespread international research efforts aimed at identifying risk and protective factors for psychopathology [15; 35]. Much of this research is summarized in Reed and colleagues’ [15; 35] Conceptual Framework to Understand the Ecological and Chronological Determinants of Mental Health in Forcibly Displaced Children (Figure 1). This ecological systems theory model [8] was empirically derived based on research with more than 11,500 youth immigrants and is a useful organizational tool for planning psychological assessments with this population. In particular, this report utilizes this model as a framework for organizing a psychodiagnostic evaluation of emotional and behavioral symptoms in youth displaced by migration.
There is a pressing need for mental healthcare among displaced youth globally. In the U.S., public policy debates surged regarding “exponential growth” in the arrival of Central American adolescents to the U.S. [36], with an estimated 131% increase between 2015 and 2016 [44]. These concerns remain, with large numbers of Central American adolescents seeking asylum in the U.S. currently. Likewise, studies of youth outside the U.S. who are displaced due to regional violence, war, economic hardship, or other danger [13; 15; 35] unequivocally reveal very elevated rates of both emotional and behavioral symptoms.Thus, it is likely that mental health practitioners will find themselves serving immigrant youth who have displayed concerning emotional and/or behavioral symptoms in the school setting; following a referral from a parent or physician; or as part of the juvenile justice system. The foundational principles of evidence-based assessment with youth certainly apply to this population and include proper documentation of informed consent and assent; assurances of confidentiality as appropriate and in compliance with mandatory reporting guidelines for abuse/neglect and danger to self/others; selection and use of evidence-based measures that have been psychometrically vetted and are appropriate in scope, language, and age-range; accurate scoring of measures given to multiple informants (e.g., youth, parent, and teacher); diagnostic formulation that considers the developmental stage of the client; and timely, written feedback in the form of an assessment report. However, beyond these standards for proper assessment, the psychodiagnostic assessment of immigrant youth requires additional consideration of their unique circumstances. In particular, the assessment should include evidence-based risk and protective factors known to be relevant to this population. In the sections that follow, these factors will be briefly reviewed, and sample measures for their assessment will be summarized.
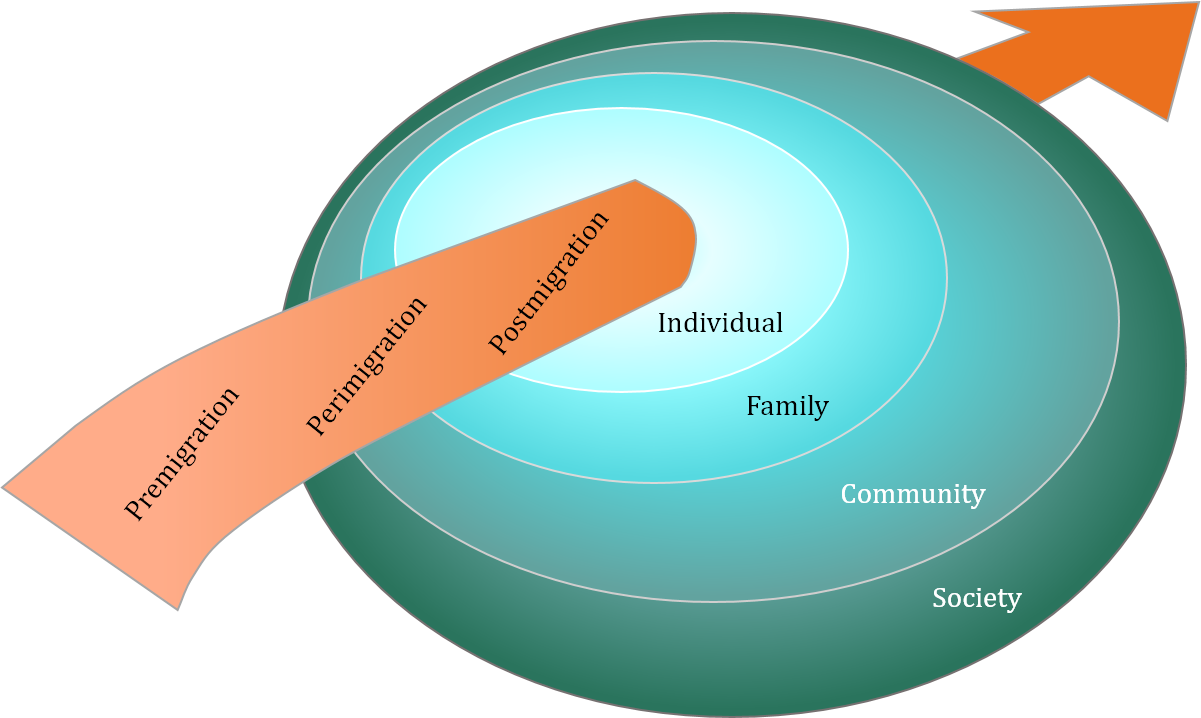
Figure 1. Reed and colleagues’ conceptual framework [34]
Evidence-Based Risk & Protective Factors
Guided by Reed and colleagues’ [15; 35] model of risk and protective factors for displaced youth, the assessment of various evidence-based risk factors should be standard in psychodiagnostic evaluation of immigrant youth. Indeed, these risk factors were selected from extant empirical research with displaced youth around the world, highlighting their importance in this population. When considering what risk factors to evaluate, clinicians should bear in mind that risk for psychopathology cuts across the individual, family, community, and societal levels and across premigration, perimigration, and postmigration stages. That is, a thorough psychodiagnostic assessment would at least screen for the possibility of, for example, exposure to violence premigration and perimigration, considering events affecting both the individual being assessed and their family members. Table 1 summarizes evidence-based risk factors to consider for inclusion in a psychodiagnostic evaluation, as well as supporting evidence.
Table 1
Reed and colleagues’risk factors for psychopathology among displaced youth and supporting empirical evidence [15; 35]
|
|
Premigration |
Perimigration |
Postmigration |
|
Individual |
Exposure to Violence |
Exposure to violence Increased age Female-Internalizing Male-Externalizing |
Increased age Female-Internalizing Male-Externalizing Educational performance [21] |
|
Family |
Exposure to violence |
Separation from caregivers |
Absence of 1+ caregiver [37; 43] Low socioeconomic status [41] |
|
Community |
|
|
Increased acculturation [38] |
Of these, it is important to note that exposure to violence and trauma affects a large number of immigrant youth and their families and is associated with significant mental health concerns as well as disruption in daily functioning for parents and youth [30; 46]. For this reason, proper assessment of both previous traumatic events, using a standardized event listvia questionnaire or interview, andsymptoms of posttraumatic stress are critical in immigrant youth. Determining how current emotional and behavioral symptoms relate temporally to traumatic exposures helps clinicians avoid confusing a posttraumatic reaction with another psychiatric illness like psychosis or developmental delay. Indeed, there are ample case examples of clinicians who have misdiagnosed immigrant youth because they failed to consider the role of trauma exposure and posttraumatic distress in shaping their clinical presentation [e.g., 29].
In addition to assessing the unique risk factors that affect immigrant youth, an informed clinician will also assess how protective factors in the premigration and postmigration environments might buffer the effects of risk factors and be capitalized upon in psychological treatment. Indeed, assessment of protective factors at all stages may also be useful for ascertaining the larger picture of immigrant youths’ functioning. Many premigration protective factors, like a secure attachment with early caregivers, may, in fact, continue to offer protection for youth, buffering the effects of risk factors or aiding in the acculturation process postmigration [46]. Based on the broader literature bases on psychopathology in African, Asian, and Central American youth, three postmigration protective factors consistently emerge and are proposed for inclusion in a thorough psychodiagnostics assessment: family functioning, peer support, and school engagement. Prior research is presented in Table 2.
Table 2
Prior Research on Protective Factors
|
Family Functioning |
Mother-child relational difficulty increased risk[1]; Unaccompanied migration increased risk [6]; Family support reduced risk[7]; Unaccompanied migration increased risk [11]; Maternal apathy increased risk [14]; Family separation increased risk [17]; Family relations associated with traumatic exposure [20]; Paternal loss increased risk [21]; Family separation or discord increased risk [22]; Low support environment and unaccompanied migration increased risk [23]; Increased parental support reduced risk [25]; Maternal communication reduced risk [32]; Family cohesion reduced risk[3], Parental loss/separation increased risk [45]; Low family connectedness increased risk [41]; Secure parental attachment reduced risk [46]; Increased parental attachment reduced risk [48] |
|
School Engagement |
Perceived school safety reduced risk [17]; Educational involvement and peer involvement reduced risk [21]; School belonging reduced risk [24]; Low neighborhood attachment, School connectedness increased risk [41]; Increased school engagement reduced risk [48] |
|
Peer Support |
Peer contact reduced risk [4]; Peer support reduced risk [7]; Social support reduced risk [14]; Peer and friend support reduced risk [25]; Increased social support reduced risk [40]; Increased peer attachment reduced risk [48] |
Sample Measures and Conclusions
Prior research clearly indicates the increased risk for psychopathology among immigrant youth and the importance of assessing a number of risk factors that are overrepresented in this population, including, among others, exposure to violence and separation from caregivers. At the same time, immigrant youth are often resilient despite exposure to staggering rates of risk, and empirical research suggests that resilience is associated with interpersonal connections in family, school, and peer contexts. With this empirical background in mind, we recommend that a psychodiagnostics assessment of emotional and behavioral symptoms in immigrant youth utilize the foundational principles of evidence-based assessment and assess the aforementioned risk and protective factors directly. Mental health screening may be undertaken using the Strengths and Difficulties Questionnaire [19], which has been translated into many languages and has undergone psychometric evaluation with multiple samples, including immigrant youth. Exposure to violence may be assessed using a questionnaire of exposure to potentially traumatic events, like the 15-item UCLA PTSD Index Trauma Screen [34] querying violent robbery, family abuse, non-family abuse, domestic violence, community violence, sexual violence, assault, and combat, as well as a posttraumatic distress measure with youth and caregiver versions like the Child PTSD Symptoms Scale [16]. Both measures can be completed in just a few minutes and have been translated into multiple languages. Importantly, published data on these instruments are lacking, although psychometric evaluation of the Child PTSD Symptoms Scale was recently undertaken by Marshall and Venta [27] with a sample of recently immigrated youth in the U.S. Separation from caregivers and other risk factors can be assessed during a semi-structured clinical interview or with an interview designed specifically for use with migrant youth [10]. Interpersonal protective factors can be assessed using a questionnaire-based measure like the Inventory of Parent and Peer Attachment[5], which is available in the public domain and has been translated into numerous languages to assess parent and peer communication, alienation, and trust and has been examined in families separated by migration [47]; a school engagement assessment (like the Engagement vs. Disaffection with Learning Scale [26]); or querying interpersonal support during a clinical interview.
By adding only a few brief questionnaires, like these, to an existing assessment battery or tailoring clinical interviewing to the aforementioned risk and protective factors, clinicians can better capture the unique risk and protective profile of immigrant youth, providing a more accurate and thorough psychodiagnostics assessment and avoiding the common pitfalls of misdiagnosis. Enhancing the evidence-based assessment of immigrant youth displaced from their homes is important given their great risk for developing emotional and behavioral symptoms and the likelihood of presenting for assessment services in school, medical, and justice settings. In this brief report, we describe unique, evidence-based risk and protective factors for psychopathology relevant to this client group based on Reed and colleagues’ [15; 35] Conceptual Framework to Understand the Ecological and Chronological Determinants of Mental Health in Forcibly Displaced Children. Adding assessment of these factors to a solid foundation of evidence-based assessment will enhance the breadth and depth of psychodiagnostic evaluations of immigrant youth.
References
-
Ajduković M., Ajduković D. Psychological well-being of refugee children. Child Abuse & Neglect, 1993, vol. 17 (6), pp. 843–854. DOI: 10.1016/s0145-2134(08)80014-2
-
Allwood M.A., Bell-Dolan D., Husain S.A. Children's trauma and adjustment reactions to violent and nonviolent war experiences. Journal of the American Academy of Child & Adolescent Psychiatry, 2002, vol. 41 (4), pp. 450–457. DOI: 10.1097/00004583-200204000-00018
-
Almqvist K., Brandell-Forsberg M. Refugee children in Sweden: Post-traumatic stress disorder in Iranian preschool children exposed to organized violence. Child Abuse & Neglect, 1997, vol. 21 (4), pp. 351–366. DOI: 10.1016/S0145-2134(96)00176-7
-
Almqvist K., Broberg A.G. Mental health and social adjustment in young refugee children 3½ years after their arrival in Sweden. Journal of the American Academy of Child & Adolescent Psychiatry, 1999, vol. 38 (6), pp. 723–730. DOI: 10.1097/00004583-199906000-00020
-
Armsden G.C., Greenberg M.T. The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence, 1987, vol. 16 (5), pp. 427–454. DOI: 10.1007/ BF02202939
-
Bean T., Derluyn I., Eurelings-Bontekoe E. et al. Comparing psychological distress, traumatic stress reactions, and experiences of unaccompanied refugee minors with experiences of adolescents accompanied by parents. Journal of Nervous and Mental Disease, 2007, vol. 195 (4), pp. 288–297. DOI: 10.1097/01.nmd.0000243751.49499.93
-
Berthold S.M. War traumas and community violence: Psychological, behavioral, and academic outcomes among Khmer refugee adolescents. Journal of Multicultural Social Work, 2000, vol. 8 (1–2), pp. 15–46. DOI:10.1300/J285v08n01_02
-
Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press, 1979. 352 p.
-
Dapo N., Kolenovic-Dapo J. Evaluation of the psychosocial adjustment of displaced children from Srebrenica. In S. Powell, E. Durakovic-Belko (eds.), Sarajevo 2000: ThePsychosocial Consequences of War: Results of Empirical Research from the Territory of Former Yugoslavia. Presentations from a Symposium Held at the Faculty of Philosophy in Sarajevo, July 7 and 8. Sarajevo: UNICEF & BH, 2002, pp. 150–154.
-
DeBrabander M., Venta A. Migration experiences of Central American youth: Developing a new measure. Psychiatry Research, 2022, vol. 314, 114652. DOI: 10.1016/ j.psychres.2022.114652
-
Derluyn I., Mels C., Broekaert E. Mental health problems in separated refugee adolescents. Journal of Adolescent Health, 2009, vol. 44 (3), pp. 291–297. DOI: 10.1016/ j.jadohealth.2008.07.016
-
Dybdahl R. Children and mothers in war: An outcome study of a psychosocial intervention program. Child Development, 2001, vol. 72 (4), pp. 1214–1230. DOI: 10.1111/1467-8624.00343
-
Ehntholt K.A., Yule W. Practitioner Review: Assessment and treatment of refugee children and adolescents who have experienced war‐related trauma. Journal of Child Psychology and Psychiatry, 2006, vol. 47 (12), pp. 1197–1210. DOI: 10.1111/j.1469-7610.2006.01638.x
-
Ekblad S. Psychosocial adaptation of children while housed in a Swedish refugee camp: Aftermath of the collapse of Yugoslavia. Stress Medicine, 1993, vol. 9 (3), pp. 159–166. DOI: 10.1002/smi.2460090306
-
Fazel M., Reed R.V., Panter-Brick C. et al. Mental health of displaced and refugee children resettled in high-income countries: Risk and protective factors. The Lancet, 2012, vol. 379 (9812), pp. 266–282. DOI: 10.1016/S0140-6736(11)60051-2
-
Foa E.B., Johnson K.M., Feeny N.C. et al. The Child PTSD Symptom Scale:
A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology, 2001, vol. 30 (3), pp. 376–384. DOI: 10.1207/S15374424JCCP3003_9 -
Geltman P.L., Grant-Knight W., Mehta S.D. et al. The “lost boys of Sudan”: Functional and behavioral health of unaccompanied refugee minors resettled in the United States. Archives of Pediatrics & Adolescent Medicine, 2005, vol. 159 (6), pp. 585–591. DOI: 10.1001/archpedi.159.6.585
-
Goldstein R.D., Wampler N.S., Wise P.H. War experiences and distress symptoms of Bosnian children. Pediatrics, 1997, vol. 100 (5), pp. 873–878. DOI: 10.1542/peds.100.5.873
-
Goodman R. The Strengths and Difficulties Questionnaire: a research note. Journal of Child Psychology and Psychiatry, 1997, vol. 38 (5), pp. 581–586. DOI: 10.1111/j.1469-7610.1997.tb01545.x
-
Grgić M., Vidović V., Soldo-Butković S. et al. Depression and perceived family functioning in Croatian displaced children. Društvenaistraživanja=Journal for General Social Issues, 2005, vol. 14, no. 3 (77), pp. 597–608.
-
Hasanoviæ M., Sinanoviæ O., Pavloviæ S. Acculturation and psychological problems of adolescents from Bosnia and Herzegovina during exile and repatriation. Croatian Medical Journal, 2005, vol. 46 (1), pp. 105–115.
-
Hjern A., Angel B., Jeppson O. Political violence, family stress and mental health of refugee children in exile. Scandinavian Journal of Public Health, 1998, vol. 26 (1), pp. 18–25.DOI: 10.1177/14034948980260010701
-
Hodes M., Jagdev D., Chandra N. et al. Risk and resilience for psychological distress amongst unaccompanied asylum seeking adolescents. Journal of Child Psychology and Psychiatry, 2008, vol. 49 (7), pp. 723–732. DOI: 10.1111/j.1469-7610.2008.01912.x
-
Kia-Keating M., Ellis B.H. Belonging and connection to school in resettlement: Young refugees, school belonging, and psychosocial adjustment. Clinical Child Psychology and Psychiatry, 2007, vol. 12 (1), pp. 29–43. DOI: 10.1177/1359104507071052
-
Kovacev L., Shute R. Acculturation and social support in relation to psychosocial adjustment of adolescent refugees resettled in Australia. International Journal of Behavioral Development, 2004, vol. 28 (3), pp. 259–267. DOI: 10.1080/01650250344000497
-
Lloyd K.S. Student engagement: Re-examining behavioral disaffection within the self-system model of motivational development. Doctoral dissertation. Tuscaloosa, AL: University of Alabama, 2014. 133 p. URL: https://ir.ua.edu/bitstream/handle/123456789/ 1963/file_1.pdf?sequence=1&isAllowed=y (Accessed: 07.06.2022)
-
Marshall K., Venta A. Psychometric evaluation of the caregiver version of the Child PTSD Symptom Scale in a recently immigrated, Spanish speaking population. Psychiatry Research, 2021, vol. 301, 113954. DOI: 10.1016/j.psychres.2021.113954
-
Mels C., Derluyn I., Broekaert E. et al. The psychological impact of forced displacement and related risk factors on Eastern Congolese adolescents affected by war. Journal of Child Psychology and Psychiatry, 2010, vol. 51 (10), pp. 1096–1104. DOI: 10.1111/j.1469-7610.2010.02241.x
-
Mercado A., Garcini L., Venta A. et al. Remain in Mexico: Trauma and abuse. Health Affairs (Millwood), 2021, vol. 40 (7), pp. 1170–1173. DOI: 10.1377/hlthaff.2020.02331
-
Mercado A., Venta A., Henderson C. et al. Trauma and cultural values in the health of recently immigrated families. Journal of Health Psychology, 2021, vol.26 (5), pp. 728–740.DOI: 10.1177/1359105319842935
-
Mollica R.F., Poole C., Son L. et al. Effects of war trauma on Cambodian refugee adolescents' functional health and mental health status. Journal of the American Academy of Child & Adolescent Psychiatry, 1997, vol. 36 (8), pp. 1098–1106. DOI: 10.1097/00004583-199708000-00017
-
Montgomery E. Trauma and resilience in young refugees: A 9-year follow-up study. Development and Psychopathology, 2010, vol. 22 (2), pp. 477–489. DOI: 10.1017/ S0954579410000180
-
Osmanović A., Zvizdić S. The effect of war-related trauma on the behaviour of adolescents. In S. Powell, E. Durakovic-Belko (eds.), Sarajevo 2000: the Psychosocial Consequences of War: Results of Empirical Research from the Territory of Former Yugoslavia.Presentations from aSymposium Held at the Faculty of Philosophy in Sarajevo, July 7 and 8. Sarajevo: UNICEF & BH, 2002, pp. 192–196.
-
Reed R.V., Fazel M., Jones L. et al. Mental health of displaced and refugee children resettled in low-income and middle-income countries: risk and protective factors. The Lancet, 2012, vol. 379 (9812), pp. 250–265. DOI: 10.1016/S0140-6736(11)60050-0
-
Rosenblum M. Unaccompanied Child Migration to the United States the Tension between Protection and Prevention, 2015. URL: http://www.migrationpolicy.org/sites/ default/files/publications/TCM-Protection-UAC.pdf (Accessed: 07.06.2022)
-
Rousseau C., Drapeau A., Platt R. Family environment and emotional and behavioural symptoms in adolescent Cambodian refugees: influence of time, gender, and acculturation. Medicine, Conflict and Survival, 2004, vol. 20 (2), pp. 151–165. DOI: 10.1080/1362369042000234735
-
Rousseau C., Drapeau A., Platt R. Living conditions and emotional profiles of Cambodian, Central American, and Quebecois youth. Canadian Journal of Psychiatry, 2000, vol. 45 (10), pp. 905–911. DOI: 10.1177/070674370004501005
-
Servan-Schreiber D., Lin B.L., Birmaher B. Prevalence of posttraumatic stress disorder andmajor depressive disorder in Tibetan refugee children. Journal of the American Academy of Child & Adolescent Psychiatry, 1998, vol. 37(8), pp. 874–879. DOI: 10.1097/ 00004583-199808000-00018
-
Shisana O., Celentano D.D. Depressive symptomatology among Namibian adolescent refugees. Social Science & Medicine, 1985, vol. 21 (11), pp. 1251–1257. DOI: 10.1016/0277-9536(85)90274-6
-
Sujoldžić A., Peternel L., Kulenović T. et al. Social determinants of health: A comparative study of Bosnian adolescents in different cultural contexts. Collegium Antropologicum, 2006, vol. 30 (4), pp. 703–711.
-
Thabet A.A.M., Vostanis P. Social adversities and anxiety disorders in the Gaza Strip. Archives of Disease in Childhood, 1998, vol. 78 (5), pp. 439–442. DOI: 10.1136/adc.78.5.439
-
Tousignant M., Habimana E., Biron C. et al. The Quebec Adolescent Refugee Project: Psychopathology and family variables in a sample from 35 nations. Journal of the American Academy of Child & Adolescent Psychiatry, 1999, vol. 38 (11), pp. 1426–1432. DOI: 10.1097/00004583-199911000-00018
-
U.S. Customs and Border Patrol. Southwest Border Sectors, 2016. URL: https://www.cbp.gov/sites/default/files/assets/documents/2016-Apr/BP%20Southwest %20Border%20Family%20Units%20and%20UAC%20Apps%20-%20Mar.pdf (Accessed: 07.06.2022)
-
Van Ommeren M., Sharma B., Komproe I. et al. Trauma and loss as determinants of medically unexplained epidemic illness in a Bhutanese refugee camp. Psychological Medicine, 2001, vol. 31 (7), pp. 1259–1267. DOI: 10.1017/S0033291701004470
-
Venta A. Attachment facilitates acculturative learning and adversity moderates: Validating the theory of epistemic trust in a natural experiment. Child Psychiatry & Human Development, 2020, vol. 51, pp. 471–477. DOI: 10.1007/s10578-020-00958-x
-
Venta A., Bailey C., Mercado A. et al. Family separation and attachment in young adults who were once left behind by caregiver migration. Psychiatry Research, vol. 302, 114039.DOI: 10.1016/j.psychres.2021.114039
-
Venta A., Bailey C., Muñoz C. et al. Contribution of schools to mental health and resilience in recently immigrated youth. School Psychology, 2019, vol. 34 (2), pp. 138–147. DOI: 10.1037/spq0000271
-
Venta A., Galicia B., Bailey C. et al. Attachment and loss in the context of US immigration: caregiver separation and characteristics of internal working models of attachment in high school students. Attachment & Human Development, 2020, vol. 22 (4), pp. 474–489. DOI: 10.1080/14616734.2019.1664604
-
Venta A.C., Mercado A. Trauma screening in recently immigrated youth: Data from two Spanish-speaking samples. Journal of Child and Family Studies, 2019, vol. 28 (1), pp. 84–90. DOI: 10.1007/s10826-018-1252-8
-
Yurtbay T., Alyanak B., Abali O. et al. The psychological effects of forced emigration on Muslim Albanian children and adolescents. Community Mental Health Journal, 2003, vol. 39 (3), pp. 203–212. DOI: 10.1023/A:1023386122344
Information About the Authors
Metrics
Views
Total: 199
Previous month: 3
Current month: 4
Downloads
Total: 80
Previous month: 0
Current month: 2